Testicular Cancer

The OHSU Knight Cancer Institute provides expert, team-based care for testicular cancer. This highly treatable cancer tends to strike younger men. We offer you:
- Doctors with advanced training and expertise in urologic and reproductive cancers
- Specialists who meet twice a month to combine their expertise patient by patient
- Oregon’s only program for patients diagnosed with cancer at ages 15 to 39
- Options to protect your fertility
- A full array of support services for you and your family
Understanding testicular cancer
The testicles are part of the male reproductive system. These two oval-shaped organs are held in a sac of skin called the scrotum, behind the penis. They make sperm cells to fertilize a female egg for pregnancy. They also make hormones such as testosterone.
What is testicular cancer?
Testicular cancer occurs when cells in the testicles grow out of control. The testicles are made up of several types of cells, which can develop into different types of cancer.
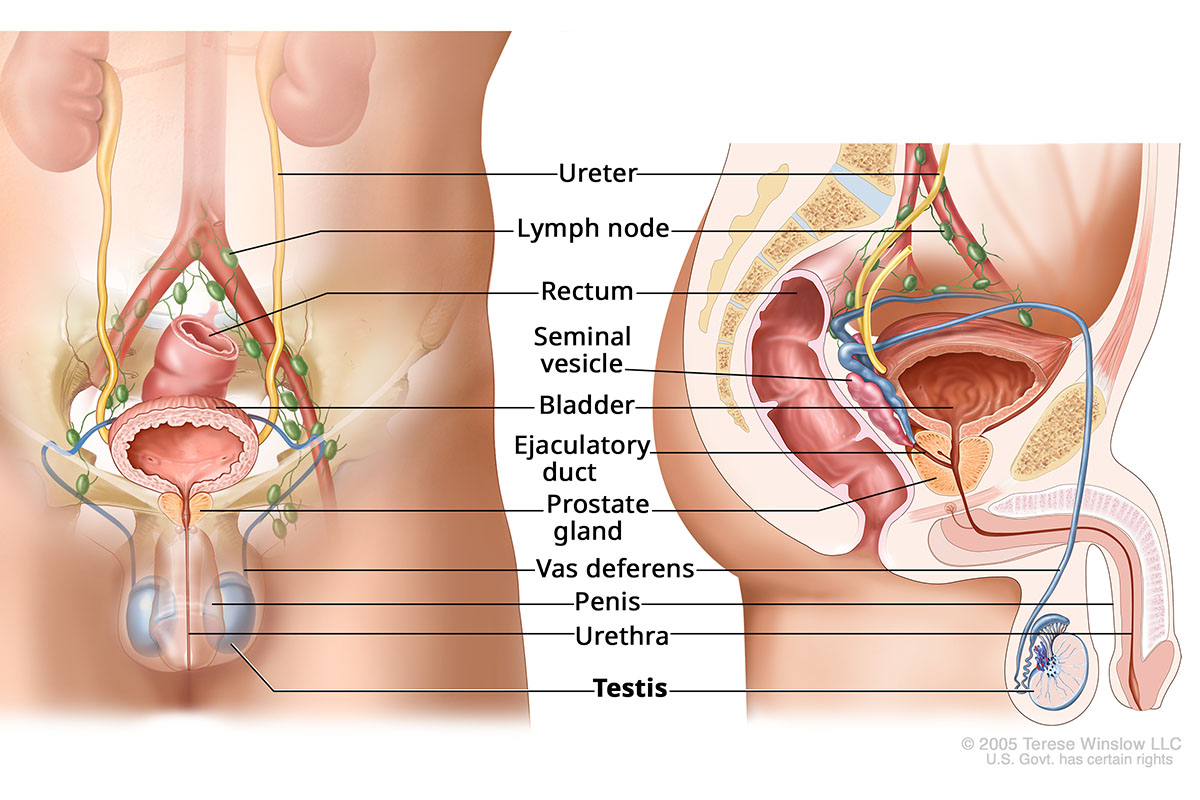
Male Genitourinary Anatomy
Who gets testicular cancer?
About 9,700 people in the U.S. are diagnosed with testicular cancer every year, according to the National Cancer Institute. About 309,000 people are living with it.
Risk factors include:
- Age: Patients tend to be younger. About half of patients are ages 20 to 34 when diagnosed. About one-quarter are ages 35 to 44.
- Race/ethnicity: White men have a much higher risk than Black men or men of Asian descent.
- Undescended testicle: People born with one or both testicles still in the abdomen are at higher risk.
- History of cancer: Men with cancer in one testicle have a higher risk of cancer in the other one.
- Family history: Having a parent or sibling with testicular cancer increases risk, though few cases overall have a family link.
- HIV infection: Risk is higher for people who have HIV (human immunodeficiency virus, the infection that causes AIDS).
- Precancerous cells: A condition called carcinoma in situ, in which abnormal cells are found in a testicle, is linked to higher risk.
Testicular cancer survival rates
The 5-year survival rate for testicular cancer is 95%. This is the portion of people, on average, still alive five years after diagnosis compared with the general population. It's important to remember that these figures are averages. They can't predict the outcome for you.
Testicular cancer symptoms
Signs of testicular cancer vary. They may be similar to those of other conditions. If you have any of these symptoms, talk with your doctor. Testicular cancer is most treatable when found early.
- A lump or fluid in the scrotum
- Pain or discomfort in the scrotum
- Sensation of heaviness in the scrotum
- Low back pain
- Chest pain or cough
- Breast tenderness or enlargement
Diagnosing testicular cancer
Screening tests may include:
Testicular exam: Your doctor will look for lumps or swelling, which could lead to more tests.
Ultrasound: This noninvasive imaging test uses sound waves to identify lumps and to see if they’re solid or fluid-filled. It can help tell cancerous cells from tumors that may not be cancer. If you have testicular cancer, your doctors may do other imaging tests to see if the cancer has spread.
Blood tests: Your doctors may be able to identify the type of cancer and its stage using a blood test. These tests look for "tumor markers," such as a high level of a protein called human chorionic gonadotropin, or HCG.
Biopsy-surgery: Your care team may want to confirm testicular cancer by looking at a tissue sample under a microscope. Unlike with many other cancers, doctors don’t use a needle or incision to get a sample because that can spread cancer cells. Instead, they remove the testicle and use follow-up tests to make sure no cancer is left.
Types of testicular tumors
If you have a testicular tumor, your doctors will identify its type to guide your treatment plan.
Germ cell tumors: Most testicular cancers arise from reproductive cells called germ cells, which make sperm. Subtypes are:
- Seminomas make up 50% of germ cell tumors. They grow relatively slowly. Nearly all patients with this type are ages 25 to 45.
- Nonseminomas are more aggressive and likely to spread. Patients with this type tend to be in their late teens to early 30s.
Stromal cell tumors: Tumors in stromal cells, which make hormones, are usually not cancer. They make up less than 5% of adult testicular tumors.
Testicular cancer stages
Determining the stage helps your care team judge how advanced your cancer is. This helps them plan the most effective treatment plan.
Cancer is only in coiled tubes called seminiferous tubules, where sperm is made.
Stage I: The tumor has grown outside the seminiferous tubules. It may have grown outside the testicle into nearby tissue. Tumor marker levels aren't available or haven’t been checked.
Stage IA: The tumor has grown outside the seminiferous tubules but is limited to the testicle. Tumor marker levels are normal.
Stage IB: The tumor has grown outside the testicle. Tumor marker levels are normal.
Stage IS: The tumor may or may not have grown outside the testicle, or it can't be measured. At least one tumor marker level is high.
Stage II: The tumor may or may not have grown outside the testicle, or it can't be measured. Cancer has spread to at least 1 nearby lymph node. Tumor marker levels aren't available or haven’t been checked.
Stage IIA: The tumor may or may not have grown outside the testicle, or it can't be measured. Cancer has spread to 1-5 nearby lymph nodes, and none is larger than 2 centimeters. Tumor marker levels are normal, or at least one is slightly higher than normal.
Stage IIB: The tumor may or may not have grown outside the testicle, or it can't be measured. Cancer has spread to at least 1 nearby lymph node that is between 2 and 5 centimeters; or it has grown beyond the lymph node; or cancer is found in more than 5 lymph nodes. Tumor marker levels are normal, or at least one is slightly higher than normal.
Stage IIC: The tumor may or may not have grown outside the testicle, or it can't be measured. Cancer has spread to at least 1 nearby lymph node that is larger than 5 centimeters. Tumor marker levels are normal, or at least one is slightly higher than normal.
Stage III: The tumor may or may not have grown outside the testicle, or it can't be measured. The cancer may or may not have spread to nearby lymph nodes. Cancer has spread to distant parts of the body. Tumor marker levels aren't available or haven’t been checked.
Stage IIIA: The tumor may or may not have grown outside the testicle, or it can't be measured. The cancer may or may not have spread to nearby lymph nodes. Cancer has spread to the lungs or distant lymph nodes. Tumor marker levels are normal, or at least one is slightly higher than normal.
Stage IIIB: One of these:
- The tumor may or may not have grown outside the testicle, or it can't be measured. The cancer has spread to 1 or more nearby lymph nodes. At least one tumor marker level is much higher than normal.
- The tumor may or may not have grown outside the testicle, or it can't be measured. The cancer may or may not have spread to nearby lymph nodes. Cancer has spread to the lungs or distant lymph nodes. At least 1 tumor marker level is much higher than normal.
Stage IIIC: One of these:
- The tumor may or may not have grown outside the testicle, or it can't be measured. The cancer has spread to 1 or more nearby lymph nodes. At least one tumor marker level is very high.
- The tumor may or may not have grown outside the testicle, or it can't be measured. The cancer may or may not have spread to nearby lymph nodes. Cancer has spread to the lungs or distant lymph nodes. At least one tumor marker level is very high.
- The tumor may or may not have grown outside the testicle, or it can't be measured. The cancer may or may not have spread to nearby lymph nodes. Cancer has spread to distant parts of the body other than the lungs or lymph nodes. Tumor marker levels may or may not be high.
Fertility preservation
If you wish to have children, our fertility experts will consult with you and your care team before treatment. You may start with cryopreservation, the long-term freezing of sperm. Removal of one testicle will not leave you infertile, but treatments such as radiation therapy and chemotherapy may damage sperm.
Testicular cancer treatments
Your care team will work with you to develop a treatment plan for your needs and wishes. Recommendations may include:
Monitoring
In some cases, we may advise closely monitoring the cancer with blood and imaging tests before deciding next steps.
Orchiectomy
Surgery to remove a testicle is called orchiectomy. It may be done as part of your diagnosis and as treatment. Your surgeon will remove the testicle and the structures that connect it to your abdomen.
Doctors make a cut in the lower abdomen to avoid touching other structures and possibly spreading the cancer. If your treatment plan calls for both testicles to be removed, we may also recommend hormone replacement to restore sexual function.
If cancer has spread to lymph nodes, these may also be removed, possibly with a minimally invasive technique. Lymph nodes, part of the immune system, are bean-size structures that filter unwanted substances.
Radiation therapy
Doctors often use radiation therapy for patients with testicular cancer. It may be used after surgery to target cancer cells that spread to nearby lymph nodes.
Options include:
- External beam radiation: A machine outside the body sends a beam of radiation to the cancer site. OHSU uses image-guided radiation therapy to precisely target cancer cells while sparing healthy tissue.
- Intensity modulated radiation therapy: IMRT is external radiation that uses computers to map the cancer in three dimensions. Radiation is shaped to the cancer, so we can deliver higher doses with less risk to normal tissue.
Chemotherapy
Chemotherapy medications kill cancer cells or stop them from reproducing. You may receive medications, alone or in combination, by mouth (as a pill or liquid) or in an IV.
Your care team may suggest chemotherapy after orchiectomy to keep cancer from coming back. Chemotherapy is also used when the cancer has spread beyond the testicle.
Stem cell transplant
If your cancer doesn't respond to conventional treatment, your doctor may recommend a bone marrow/stem cell transplant. This gives your immune system new, healthy cells to help you fight the disease.
Reconstructive surgery
If you have a testicle removed, you may be a candidate for reconstructive surgery to replace it with a prosthetic (artificial) one. Your urologist can discuss this option with you and your care team.
More OHSU services
- Our Adolescent and Young Adult Oncology Program provides support and other services for young people coping with cancer. The program’s director, Dr. Brandon Hayes-Lattin, survived testicular cancer after being diagnosed at age 28.
- The Knight Cancer Institute is at the forefront of research into promising new cancer treatments. Look for an OHSU clinical trial for testicular cancer.
- Scientists at our Cancer Early Detection Advanced Research Center, or CEDAR, are finding new ways to identify cancer when it’s most treatable.
Learn more
- Testicular Cancer, National Cancer Institute
- Testicular Cancer, American Cancer Society
Testicular Cancer team
-
- Christopher Amling, M.D., F.A.C.S
- Accepting new patients
-
- Jennifer Botelho, MPAS, PA-C (she/her)
- Accepting new patients
-
- Jeremy Paul Cetnar, M.D., M.S.H.P.R.
- Accepting new patients
-
- Mark Garzotto, M.D.
- Accepting new patients
-
- Brandon Hayes-Lattin, M.D., FACP
- Accepting new patients
-
- Sudhir Isharwal, M.D., M.B.A.
- Accepting new patients
-
- Ryan Kopp, M.D.
- Accepting new patients
-
- Lisa Langmesser, MHS, PA-C
- Accepting new patients
-
- Jen-Jane Liu, M.D.
- Accepting new patients
-
- Ronald Ng, M.D. (he/him)
- Accepting new patients
-
- Max Poole, PA-C (he/him)
- Accepting new patients
-
- Christopher W. Ryan, M.D.
- Accepting new patients
-
- Hilary Shreves, M.S.N., A.C.N.P.-B.C.
- Accepting new patients
-
- Marshall Strother, M.D.
- Accepting new patients
-
- Jacqueline Vuky, M.D.
- Accepting new patients
-
- Casey Williamson, M.D., M.A.S. (he/him)
- Accepting new patients
Location
Knight Cancer Institute, South Waterfront
Center for Health & Healing, Building 2
3485 S. Bond Ave.
Portland, OR 97239
Free parking for patients and visitors
Refer a patient
- Refer your patient to OHSU.
- Call 503-494-4567 to seek provider-to-provider advice.
Cancer clinical trials
Clinical trials allow patients to try a new test or treatment.
Read more
Learn more about OHSU Knight Cancer Institute treatments:
Stay informed
News: Read about research breakthroughs, patient care and many other topics on our OHSU News site.