Cervical Cancer

Cervical cancer forms in the cervix, the lower part of the uterus that connects to the vagina.
The OHSU Knight Cancer Institute provides sensitive, expert care for people dealing with cervical cancer. You’ll find:
- Team-based care, with specialists who work with you on the best treatment plan
- Screening and treatment for changes in the cervix that increase cancer risk
- Support services, including options for fertility after cancer
- Clinical trials to develop new treatments for cervical cancer
What is cervical cancer?
Anatomy of the Cervix
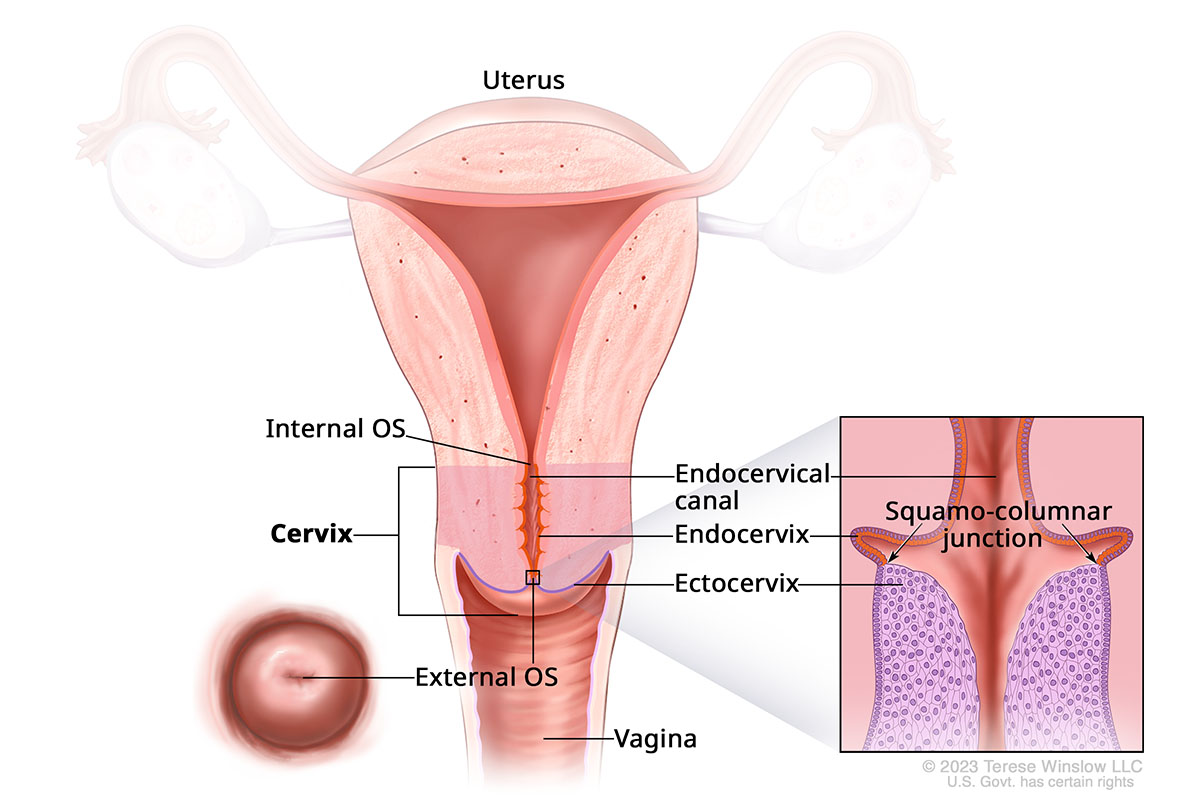
The cervix is a tiny organ shaped like a cylinder. It connects the bottom of the uterus and the top of the vagina. Cervical cancer starts when cells in the cervix grow out of control.
Almost all cervical cancers are caused by certain types of the human papilloma virus, or HPV. The HPV vaccine can often prevent cervical cancer. Regular screening can detect cervical cancer early, when it has a high survival rate.
Cervical cancer types
Squamous cell carcinoma: This makes up about 70% of cervical cancers. It starts in the cells lining the part of the cervix at the top of the vagina.
Adenocarcinoma: This forms in the cells that line the cervical canal, or the passage between the vagina and uterus.
Who gets cervical cancer?
About 13,300 new cases of cervical cancer are diagnosed in the U.S. every year, according to the National Cancer Institute. Roughly 298,000 people in the U.S. are living with the condition.
Risk factors
Anyone with a cervix is at some risk. Risk factors include:
Anything that makes it more likely for someone to be infected by HPV: Human papilloma virus spreads mostly through sex. The risk is higher for people who have sex at a young age or have many sex partners. HPV infections are common and often go away by themselves. When certain HPV infections persist, they can cause cancer.
Anything that makes it harder for the immune system to fight HPV: This includes smoking. Women who smoke have double the risk of cervical cancer.
Lack of access to health care: People who aren’t getting Pap tests, HPV tests or other cervical screening are at higher risk. Screening tests can find abnormal cells before they turn into cancer.
Exposure to diethylstilbestrol, or DES: DES was once given to pregnant women in the United States to prevent miscarriage. Exposure to DES in the womb can increase risk for some types of rare cervical cancer.
Survival rates
The five-year relative survival rate for cervical cancer is 68%, according to the National Cancer Institute. This is the portion of people who are alive five years after diagnosis compared with the general population. The rate rises to 91% if cervical cancer is found in the earliest stage.
It’s important to remember that survival rates are averages. They can't predict your outcome.
Cervical cancer signs and symptoms
Early cervical cancer usually has no symptoms. It’s mostly found through a screening test.
In later stages, symptoms may include:
- Bleeding between periods, after sex or after menopause
- Unusual vaginal discharge, sometimes with blood
- Pelvic pain or pain during sex
- Trouble peeing
- Blood in the urine
- Swollen legs
These symptoms may have other causes. It’s best to tell your doctor if you have symptoms so you can get the right care.
Cervical cancer screening
Cervical cancer is one of the most preventable cancers. Screening tests can find cancer early, when it’s easier to treat.
Pelvic exam: Your doctor will examine the pelvic organs from the outside and through the vagina.
Pap test: Your doctor will gently scrape or brush some cells from the cervix to look at under a microscope.
HPV test: Cells from the cervix are checked for high-risk types of HPV.
If you are 30 or older, you may have more risk of a long-lasting HPV infection. A Pap test combined with an HPV test can help find early cervical cancer.
Cervical cancer diagnosis
If your doctor thinks you may have cervical cancer, you may have one of these tests:
Colposcopy: This uses a magnifying device called a colposcope to look for cell changes on the cervix. Your doctor might do a biopsy at the same time. That means removing a bit of tissue to look at under a microscope.
Endocervical curettage: This uses a small spoonlike instrument called a curette. Your doctor will remove a bit of tissue from inside the cervix to look at under a microscope.
LEEP (loop electrosurgical excision procedure): This uses a thin wire loop with an electrical current to gently cut away abnormal tissue.
Cone biopsy: This removes a cone-shaped sample of tissue from the cervix. It helps your doctor check for cell changes or abnormal cells deeper in the cervix. It is usually done with anesthesia in an operating room.
Imaging: If you get a diagnosis of cervical cancer, your doctor may order an X-ray or MRI, CT or PET scan. This helps your care team see where the cancer is and whether it has spread.
Cervical cancer stages
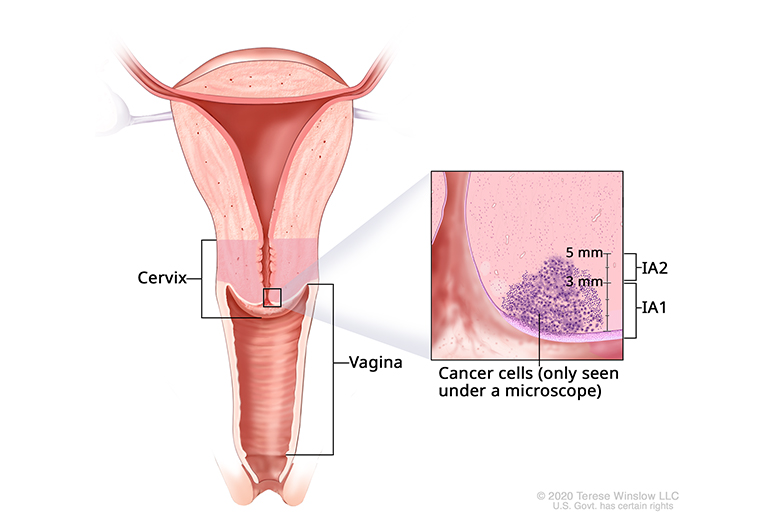
Stage IA Cervical Cancer
Doctors use stages to describe whether cancer has spread and how far. Cervical cancer stages range from I to IV (4). Generally, the higher the number, the more the cancer has spread.
Staging can be complex and vary from person to person. It’s best to talk with your doctor about your stage.
Stage I: The cancer is only in the cervix.
Stage II: The cancer has spread beyond the cervix and uterus. It has not spread to the pelvis, vagina, nearby lymph nodes or distant parts of the body.
Stage III: The cancer has spread to the lower vagina or to the pelvis. The cancer may have spread to nearby lymph nodes. It may block the tubes that carry urine from the kidneys to the bladder.
Stage IV: The cancer has spread to the bladder, rectum or outside the pelvic area.
Cervical Cancer, Stage1A1 and 1A2
Cervical cancer treatment
For early cervical cancer, you may have only surgery. We offer robotic surgery for a more precise operation and a faster recovery.
For cancer that has spread outside the cervix, you may have radiation therapy and chemotherapy.
Surgery
Cone biopsy: This removes a cone-shaped piece of cervical tissue. A cone biopsy may allow patients to keep the ability to get pregnant.
Trachelectomy: This removes the cervix but leaves the rest of the uterus.
Hysterectomy: This removes the cervix and uterus. Sometimes the ovaries, fallopian tubes and nearby lymph nodes also are removed.
Radiation therapy
Radiation therapy uses beams of energy to target cancer cells. It is often used for cervical cancer that has spread to nearby tissue. Radiation therapy is also often used with chemotherapy.
External beam radiation: This uses a machine outside the body to send radiation to the pelvis.
Brachytherapy: This delivers radiation inside the body, with a device placed in or near the cervix.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells or stop their growth.
For cervical cancer, cisplatin is often used along with radiation therapy. Chemotherapy may also be used for advanced cervical cancer or cervical cancer that comes back.
Targeted therapy
Targeted therapy uses drugs to attack cancer cells while avoiding healthy cells.
For advanced cervical cancer or cervical cancer that comes back, a drug called Avastin (bevacizumab) is sometimes added to chemotherapy. Avastin is given in an IV drip.
Immunotherapy
Immunotherapy helps your immune system find and attack cancer cells.
Keytruda (pembrolizumab) is approved for cervical cancers that have:
- Spread
- Come back and test positive for a certain protein
- Certain genetic changes that may affect how they respond to treatment
Dr. Amanda Bruegl: A patient's view
Learn more
- What is Cervical Cancer? National Cancer Institute
- Cervical Cancer, American Cancer Society
- HPV and Cancer, National Cancer Institute
Cervical cancer team
Gynecologic oncologists
-
- Amanda Bruegl, M.D. (she/her)
- Accepting new patients
-
- Amanda J. Compadre, M.D. (she/her/ella)
- Accepting new patients
-
- Ross Harrison, M.D., M.P.H. (he/him)
- Accepting new patients
-
- Breana L. Hill, M.D. (she/her)
- Accepting new patients
-
- Jessica Jou, M.D., M.S., FACOG (she/her)
- Accepting new patients
-
- Elizabeth Munro, M.D.
- Accepting new patients
Radiation oncologists
-
- Cheryl Claunch, M.D., Ph.D. (she/her)
- Accepting new patients
-
- Casey Williamson, M.D., M.A.S. (he/him)
- Accepting new patients
Location
Knight Cancer Institute, South Waterfront
Center for Health & Healing, Building 2
3485 S. Bond Ave.
Portland, OR 97239
Free parking for patients and visitors
Cancer clinical trials
Clinical trials allow patients to try a new test or treatment.