Anal Cancer
At the OHSU Knight Cancer Institute, you receive care for anal cancer from a team of specialists. We offer you:
- Surgeons skilled in minimally invasive surgery and tissue-sparing options.
- The only team-based program for anal cancer in Oregon.
- Treatments you won't find elsewhere in the region.
- HRA (high-resolution anoscopy) to catch cancers and pre-cancers early.
- Hundreds of clinical trials for early access to promising treatments.
- Social workers, dietitians and other cancer experts to support you.
Understanding anal cancer
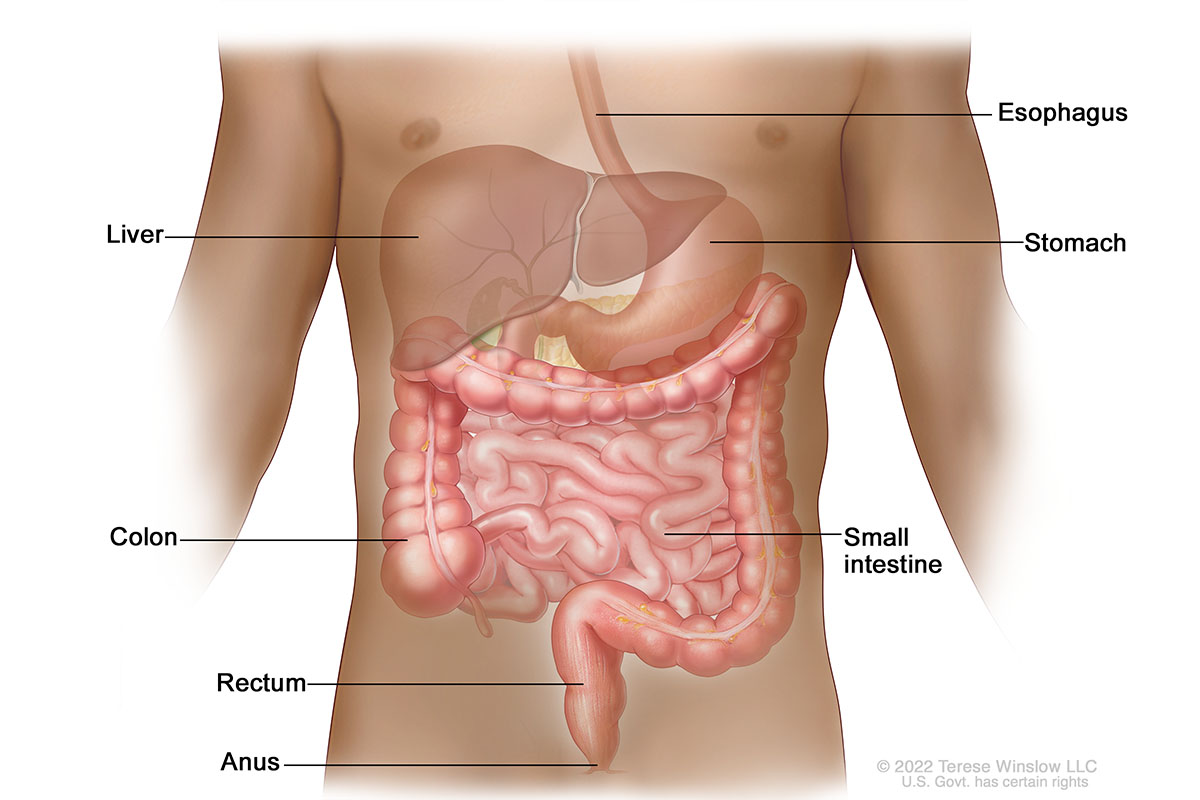
Lower Gastrointestinal Anatomy
What is anal cancer?
The anus is the last part of the bowel or large intestine, after the rectum. It is about 1.5 inches long. When we digest food, the solid waste, or stool, exits the body through the anus. Anal cancer happens when abnormal cells grow in the tissue lining the anus. Most anal cancers are caught early, when they’re most treatable.
Who gets anal cancer?
Anal cancer is rare. About 11,000 people in the U.S. are diagnosed with anal cancer every year, according to the National Cancer Institute, and 85,700 people are living with it.
Risk factors include:
- Age: Anal cancer is more common in people ages 55 to 64.
- Gender: It’s more common in women, though that can vary by race and ethnicity. For instance, Black men are more likely to get anal cancer than Black women, at least before age 60.
- Health history: Having a condition such as HPV (human papillomavirus) or HIV (human immunodeficiency virus) can weaken your body’s natural defenses, increasing risk. Women with certain reproductive cancers (cervical, vulvar or vaginal) may also be at higher risk.
- Immunosuppression: Some people, such as transplant patients or patients with inflammatory bowel disease, take drugs to suppress their immune system. These drugs can raise your risk of anal cancer.
- Sexual history: Having multiple partners, anal sex or unprotected sex increases risk of HPV, HIV and other infections linked to anal cancer. Men who have sex with men are also at higher risk.
- Smoking: Smokers are at higher risk.
Survival rates for anal cancer
A key concept in understanding survival is five-year relative survival rate. This is the percentage of people who are still alive five years after they were first diagnosed, compared to the general population. (It doesn’t count death from other causes.)
The five-year relative survival rate for anal cancer is 71%, according to the National Cancer Institute. The rate is 85% if the cancer is caught early.
It's important to remember that survival rates are averages and can't predict the outcome for any one patient. It's also important to know that they are based on the treatments available more than five years ago. Patients who are diagnosed now may have a better outlook. Treatments are getting better all the time.
What causes anal cancer?
HPV (human papillomavirus) causes more than 90% of anal cancers, according to the National Cancer Institute. This virus spreads through skin-to-skin contact, including sexual activity. The virus can cause warts to form in the lining of the anus or on the skin outside the anus. These warts increase the risk of anal cancer.
The warts start out about the size of pinheads, so you may not notice them at first. Many people have no symptoms of an HPV infection until it progresses to a more serious condition such as anal cancer.
For women, screening tests normally done at the same time as a cervical cancer screening test (Pap smear) detect HPV. There is no HPV screening test for men. A vaccine for children and young adults (ages 9 to 26 but usually recommended at age 11 or 12) protects against HPV.
Anal cancer symptoms
Bleeding from the anus or rectum is an early symptom but can also be from hemorrhoids (swollen veins near the anus) or another condition. It’s important to talk with your doctor if symptoms such as rectal bleeding persist.
Other symptoms include:
- Discharge from the anus such as pus or mucus.
- Changes in bowel movements, such as narrow stools.
- Itching near the anus that doesn’t stop.
- Pain or pressure near the anus.
- Swelling or a mass in the anus or nearby tissue.
Types of anal cancer
The two most common forms of anal cancer are:
- Squamous cell carcinoma, which affects the cells lining the surface of the anus. This type accounts for nearly 90% of anal cancers.
- Adenocarcinoma, which starts beneath the surface of the anus. This type affects cells that make mucus to lubricate the anus.
Other conditions include:
- Rare forms of anal cancer include basal cell carcinoma and melanoma.
- Anal intraepithelial neoplasia (precancerous cells) can occur when epithelial (skin) cells in the anus develop unusual features or form growths.
Diagnosing anal cancer
Our team will do a thorough physical exam and tests that may include:
- Digital rectal exam: Your doctor will use a gloved, lubricated finger to carefully feel the anus for warts or other masses.
- Anal Pap smear: We collect a cell sample by gently scraping the anus with a plastic tool. We look at the cells under a microscope to check for signs of cancer.
- Anoscopy: We use a short, hollow tube with a light, called an anoscope, to look at the lining of the anus. We can use a tool at the tip to take a tissue sample, called a biopsy, to examine under a microscope.
- Proctoscopy: This test, similar to anoscopy, uses a longer tool called a proctoscope to see the far end of the anus and the rectum.
- CT scan: This test uses X-rays to create 3D images of the anus to check for signs of cancer. Air is pumped in to expand the tissues for better images.
- MRI scan: Radio waves and a large magnet create images of structures inside the body. The Knight Cancer Institute is the only center in Oregon with a 3 Tesla MRI to show small areas in great detail.
High-resolution anoscopy (HRA)
High-resolution anoscopy (HRA) is an important tool in diagnosing anal cancers and pre-cancers.
Your team uses a powerful microscope to look inside the anal canal. They focus on an area about an inch inside the canal where two types of cells meet. Starting at the opening, the canal is lined with skin cells. Further inside, the canal is lined with mucous cells. The cells meet in a zone called the squamous epithelial junction. Most anal cancers and pre-cancers arise in this area.
In HRA, your team looks closely at the junction for signs of abnormal cells, also known as anal dysplasia. Doctors divide these abnormal cells into four types:
- Low-grade squamous intraepithelial lesions (LSIL): The cells look slightly different from normal. This is not cancer. You probably don’t need treatment but you should come back for monitoring.
- High-grade squamous intraepithelial lesions (HSIL): The cells look more different. This is not cancer, but it turns into cancer in a small portion of cases. You may need the lesions removed.
- Anal carcinoma in situ: These are cancer cells on the surface of the anal canal.
- Squamous cell carcinoma: These are cancer cells that have spread beyond the surface.
Find out more about HRA and make an appointment at the OHSU Digestive Health Center.
Anal cancer stages
Your team will assign a stage to your tumor. The stage indicates how advanced your tumor is and how fast it’s likely to grow.
Tumor Sizes
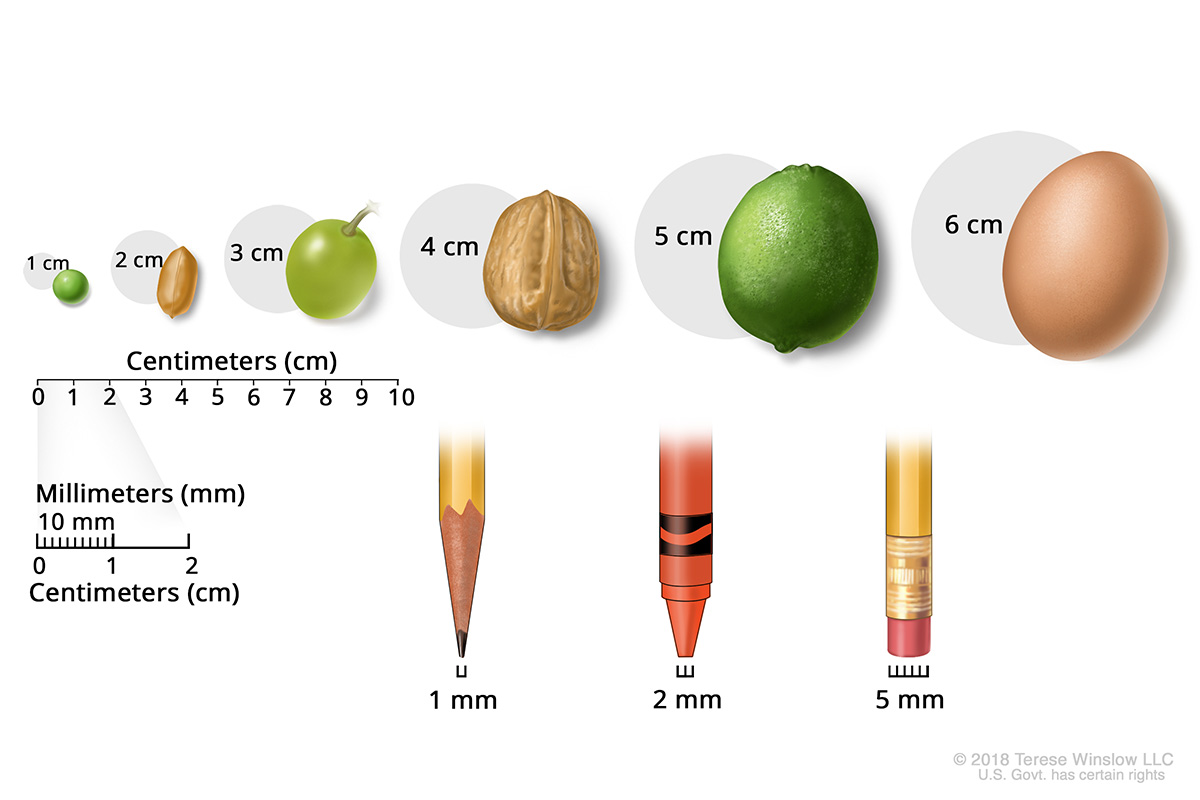
Stage I: The tumor is 2 centimeters or less.
Stage II:
- Stage IIA: The tumor is larger than 2 centimeters but not more than 5 centimeters.
- Stage IIB: The tumor is larger than 5 centimeters.
Stage III:
- Stage IIIA: The tumor is no larger than 5 centimeters, and cancer has spread to lymph nodes near the rectum. These bean-size structures act as filters for the immune system.
- Stage IIIB: Cancer has spread to nearby organs, such as the bladder, prostate gland or vagina.
- Stage IIIC: The tumor is larger than 5 centimeters, and cancer has spread to the lymph nodes near the rectum. Or the tumor is any size, and cancer has spread to nearby organs and lymph nodes.
Stage IV: Cancer has spread to distant parts of the body such as the liver or lungs.
Coordinated care
Our gastrointestinal cancer experts work together to recommend a treatment plan for your individual needs. We gather weekly in a meeting called a tumor board, pooling our expertise for every anal cancer patient. Our specialists include:
- Gastroenterologists, who do first evaluations and may remove early-stage cancers.
- Surgeons, who specialize in complex pelvic procedures, including anal cancer care.
- Medical oncologists, who treat cancer using medications.
- Radiation oncologists, who treat cancer using radiation therapy.
- Radiologists, who do imaging tests to see a tumor’s size and location.
- Pathologists, who study tissue samples (biopsies) under a microscope to make or confirm a diagnosis.
Anal cancer treatment
Your treatment depends on the size and stage of your tumor.
Surgery for early tumors
For early tumors (stage 0 or I), our surgeons may be able to remove the cancer with a surgery called local resection (also known as wide local excision). This minimally invasive technique is designed to spare tissue and save the sphincter muscle.
Chemoradiation
Chemoradiation pairs chemotherapy and radiation therapy. Studies show that it’s highly effective in treating anal cancer. It is sometimes called the Nigro Protocol after the doctor who developed it.
Chemoradiation at the Knight Cancer Institute generally begins with a round of chemotherapy in an IV drip. Then patients receive intensity-modulated radiation therapy, which uses high-powered beams of energy to attack cancer cells. After that, patients receive another round of chemotherapy. The entire course of treatment lasts about six weeks.
About 70-80% of tumors treated with chemoradiation disappear.
Surgery for more advanced tumors
The surgery for more advanced tumors is called abdominoperineal resection. Surgeons remove the anus, rectum and a section of colon. Next they create an opening (stoma) in your belly and connect it to your colon. This procedure is called a colostomy. The stoma will connect to an ostomy bag outside your body to collect stool.
Ostomy care
Our team includes nurses with special training to help you overcome fears, find ostomy products, and learn to care for your ostomy. An ostomy won’t keep you from doing sports or other activities you enjoy.
Monitoring
Because anal cancer can come back, your care team will schedule regular follow-up visits. This enables us to detect the earliest signs of cancer, giving you the best chance for successful treatment.
Anal cancer team
Surgery
-
- Robert L. Eil, M.D.
- Accepting new patients
-
- Sandy H. Fang, M.D., FACS, FASCRS (she/her)
- Accepting new patients
-
- Daniel O. Herzig, M.D., M.B.A., FACS, FASCRS (he/him)
- Accepting new patients
-
- Rodney F. Pommier, M.D., FACS, FSSO
- Accepting new patients
-
- Flavio G. Rocha, M.D., FACS, FSSO
- Accepting new patients
-
- Divya Sood, M.D.
- Accepting new patients
-
- V. Liana Tsikitis, M.D., M.B.A., M.C.R., FACS, FASCRS (she/her)
- Accepting new patients
-
- Patrick J. Worth, M.D., M.C.R., FACS, FSSO (he/him)
- Accepting new patients
Medical oncology
-
- Emerson Y. Chen, M.D.
- Accepting new patients
-
- Jeff Donovan, PA-C
- Accepting new patients
-
- Adel Kardosh, M.D., Ph.D.
- Accepting new patients
-
- Guillaume Pegna, M.D.
- Accepting new patients
Radiation oncology
-
- Nima Nabavizadeh, M.D.
- Accepting new patients
Medical genetics
-
- Kelly Jo Hamman, M.S., CGC
- Accepting new patients
Learn more
- Anal Cancer, National Cancer Institute
- Anal Cancer, American Cancer Society
- Living with Anal Cancer, Anal Cancer Foundation
Location
Knight Cancer Institute, South Waterfront
Center for Health & Healing, Building 2
3485 S. Bond Ave.
Portland, OR 97239
Free parking for patients and visitors
Refer a patient
- Refer your patient to OHSU.
- Call 503-494-4567 to seek provider-to-provider advice.
Cancer clinical trials
Clinical trials allow patients to try a new test or treatment.
Read more
Learn more about OHSU Knight Cancer Institute treatments:
Stay informed
News: Read about research breakthroughs, patient care and many other topics on our OHSU News site.