Vaginal, Vulvar and Rare Gynecologic Cancers
Vaginal and vulvar cancers are rare cancers of the female reproductive system. They can often be cured when found and treated early.
Your care team at the OHSU Knight Cancer Institute will work with you on a care plan for your needs. You’ll find:
- The latest technology to find and treat cancer
- Surgeons with experience in restoring the vulva and vagina
- Nurses who guide you through your care
- Support services, including help for fertility after cancer
What are vaginal and vulvar cancers?
Anatomy of the Female Reproductive System
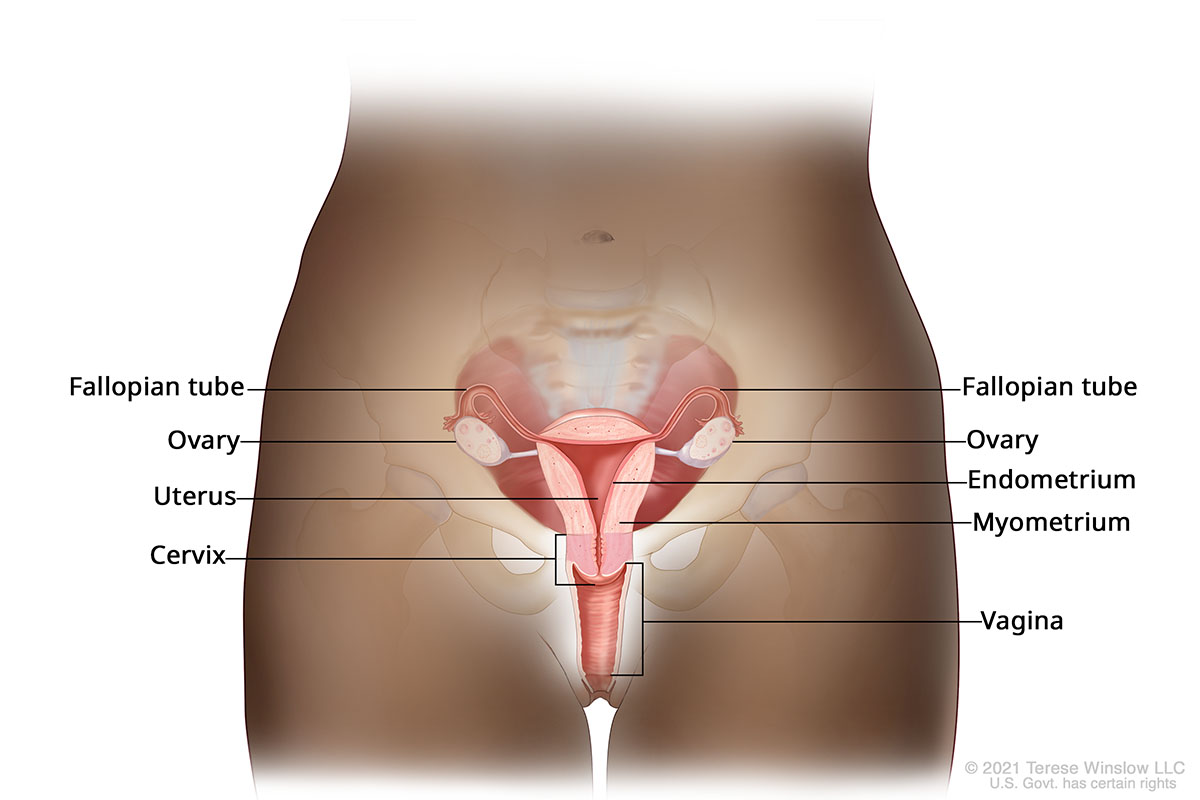
Vaginal, vulvar and other rare gynecologic cancers form when cells grow out of control.
Vaginal cancer: This starts in the vagina.
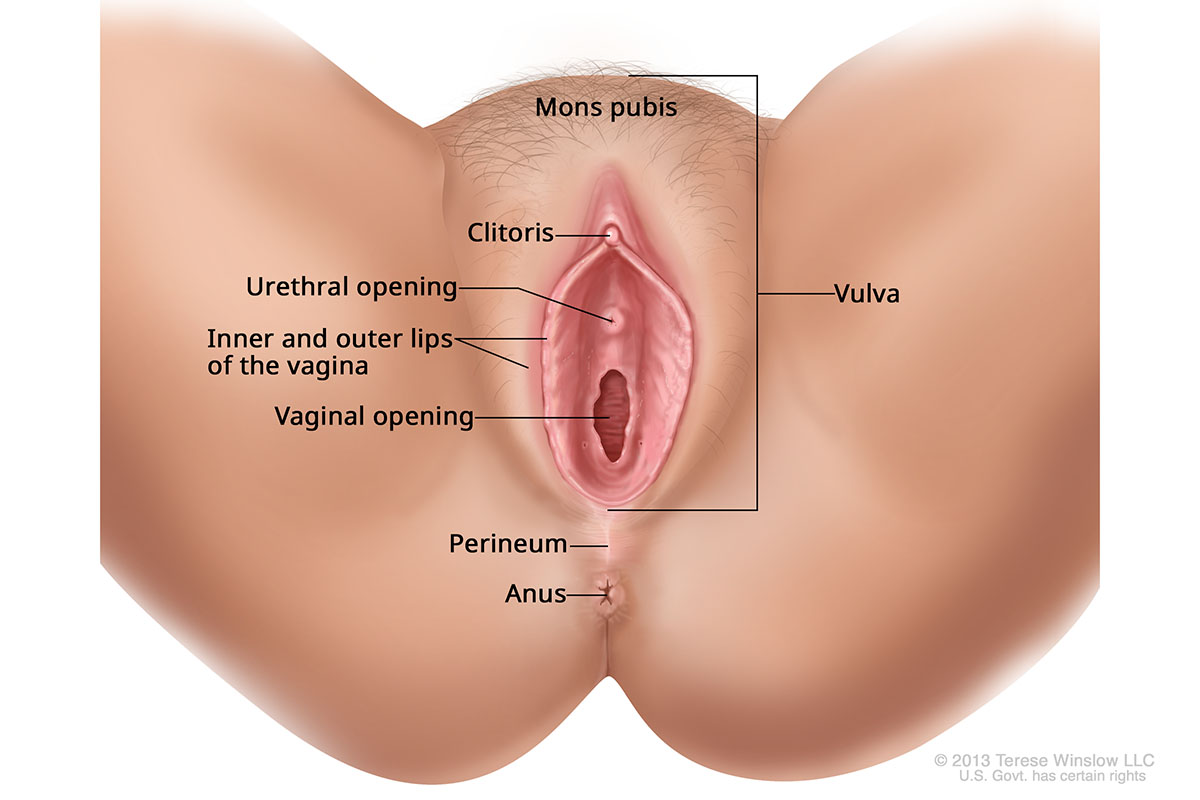
Vulvar cancer: This starts in the folds around the vagina’s opening. Cancer is found most often on the inner edges of the labia. It is sometimes found on the clitoris or in the vulva’s glands.
Anatomy of the Vulva
Types of gynecologic cancers
Squamous cell carcinoma: This makes up 85% to 90% of vaginal and vulvar cancers.
Adenocarcinoma: This forms in the mucus cells and glands of the vagina and vulva.
Other rare gynecological cancers:
Who gets vaginal and vulvar cancers?
Vaginal cancer: About 8,000 people are diagnosed with vaginal cancer in the U.S. every year, according to the National Cancer Institute.
Vulvar cancer: About 7,480 people are diagnosed with vulvar cancer in the U.S. every year, according to the National Cancer Institute.
Risk factors
Anyone with a vulva or vagina is at some risk. Risk factors include:
Age: People 60 and older are most likely to develop these cancers. Risk rises with age.
A history of:
- HPV (human papillomavirus) infection
- Cervical cancer or other cancers of the female reproductive system
- Genital warts
- Hysterectomy
- Abnormal cells
- Smoking
- HIV infection
For vaginal cancer: Diethylstilbestrol, or DES, was once used in the U.S. to prevent miscarriage. Exposure to DES in the womb raises risk.
Survival rates
The five-year relative survival rate for vulvar cancer is 70%, according to the National Cancer Institute. This rises to 86% if the cancer is found early.
The five-year relative survival rate for vaginal cancer is 76% if the cancer is found early.
Five-year survival rate is the portion of people alive five years after diagnosis, compared with the general population. It’s important to remember that survival rates are averages. They don’t predict the outcome for any one person.
Vaginal and vulvar cancer signs and symptoms
Vaginal and vulvar cancers often have no early signs or symptoms.
If you do have symptoms, they can include:
- Unusual bleeding or discharge
- Sores, lumps or growths
- Itching or burning
- Tenderness or pain, especially during sex or peeing
- Changes in skin color
- Constipation, or bowel or urine changes
- Swollen belly
These symptoms may have other causes. It’s best to tell your doctor about symptoms so you can get the right care.
Vaginal and vulvar cancer diagnosis
If your doctor thinks you may have vaginal or vulvar cancer, you may have any of these tests:

Pelvic exam: Your doctor inspects your vagina and vulva with their eyes, hands and a tool called a speculum.
Pap smear: Your doctor takes a bit of tissue from your cervix to look at under a microscope.
Colposcopy: This uses a magnifying device to look for suspicious tissue. The doctor may also take a tissue sample for testing (biopsy).
Biopsy: This takes a bit of tissue to look at under a microscope.
Imaging: This uses scans to look for cancer and see if it has spread.
Vaginal and vulvar cancer stages
Doctors use stages to describe how much cancer is in the body and how much it has spread.
Vaginal and vulvar cancer stages go from stage I through IV (4). Generally, a higher number means the cancer has spread more.
Staging is complex and varies from person to person. It’s best to talk with your doctor about your stage.
Vaginal cancer
Stage I: The cancer is only in the vagina.
Stage II: The cancer has grown through the vaginal wall.
Stage III: The cancer may be growing into the pelvic wall. Or it may be blocking the flow of urine, which means the kidneys can’t work. The cancer may be in nearby lymph nodes.
Stage IV: The cancer has spread to the bladder or rectum, or is growing outside the pelvis. Or it has spread to distant organs. It may be in nearby lymph nodes.
Vulvar cancer
Stage I: The cancer is in the vulva, perineum (the tissue between the rectum and vagina) or both. It has grown into underlying tissue.
Stage II: The cancer is growing into the lower third of the anus, vagina or urethra, the tube that drains urine (pee) from the bladder.
Stage III: The cancer is in the upper two-thirds of the vagina or urethra, or in the lining of the bladder or rectum. Or it has spread to nearby lymph nodes.
Stage IV: The cancer is in pelvic bone or has attached to underlying tissue or caused a sore on at least one lymph node. Or it has spread to distant organs.
Vaginal and vulvar cancer treatment
Your care team will work with you on a plan tailored to your diagnosis, health and desire to have children.
Surgery
Surgery removes as much of the cancer as possible. We use robotic surgery for less pain, smaller cuts and quicker recovery. We may use a laser to remove abnormal tissue that isn’t cancer.
Chemotherapy
Chemotherapy uses drugs to kill or stop the growth of cancer cells. Chemo may be used with radiation therapy. Chemo can be used to:
- Shrink a tumor before surgery
- Kill cancer cells that remain after surgery
- Slow the growth and control the symptoms of advanced cancer
Radiation therapy
Radiation therapy uses beams of energy to damage or destroy cancer cells before or after surgery.
External beam radiation: This uses a machine outside your body.
Brachytherapy: This uses radioactive seeds that are placed in the vagina for a short time to deliver radiation to the tumor.
Reconstructive surgery
Reconstructive surgery helps restore the look and function of the vagina or vulva. Our plastic and reconstructive surgery team has expertise in this delicate surgery.
Learn more
- Vaginal cancer, American Cancer Society
- Vulvar cancer, American Cancer Society
- Gestational trophoblastic disease, National Cancer Institute
Vaginal and vulvar cancer team
Gynecologic oncologists
-
- Amanda Bruegl, M.D. (she/her)
- Accepting new patients
-
- Amanda J. Compadre, M.D. (she/her/ella)
- Accepting new patients
-
- Ross Harrison, M.D., M.P.H. (he/him)
- Accepting new patients
-
- Breana L. Hill, M.D. (she/her)
- Accepting new patients
-
- Jessica Jou, M.D., M.S., FACOG (she/her)
- Accepting new patients
-
- Elizabeth Munro, M.D.
- Accepting new patients
Radiation oncologists
-
- Cheryl Claunch, M.D., Ph.D. (she/her)
- Accepting new patients
-
- Casey Williamson, M.D., M.A.S. (he/him)
- Accepting new patients
Location
Knight Cancer Institute, South Waterfront
Center for Health & Healing, Building 2
3485 S. Bond Ave.
Portland, OR 97239
Free parking for patients and visitors
Cancer clinical trials
Clinical trials allow patients to try a new test or treatment.
Read more
Learn more about OHSU Knight Cancer Institute treatments:
Stay informed
News: Read about research breakthroughs, patient care and many other topics on our OHSU News site.