Understanding Melanoma
Melanoma is the least common skin cancer but the most important to catch early. It’s almost always curable when found early, but it can become deadly if allowed to spread. Important things to know:
- Melanoma must be taken seriously. It is more likely than other skin cancers to spread.
- Exposure to ultraviolet rays, from the sun or tanning beds, is a main cause of melanoma.
- Oregon has a high rate of melanoma cases compared with other states.
- Rates have been increasing for the past four decades.
- Melanoma can strike anyone but is much more common in white people.
- Melanoma is more common in older people but is also one of the most common cancers among young adults.
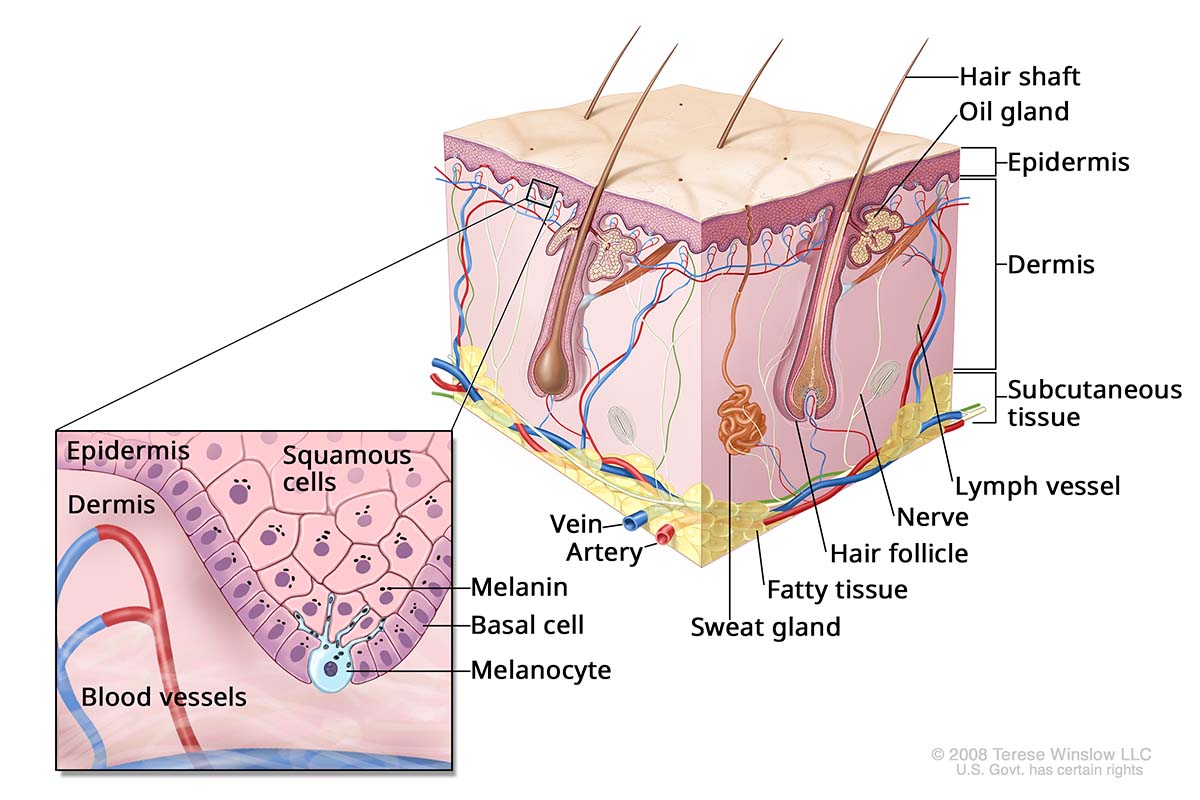
What is melanoma?
Melanoma is a type of cancer that arises from pigmented cells called melanocytes. It most often occurs in melanocytes in the skin’s top layer. Less often, melanomas form in other parts of the body, such as the eyes and mouth.
Skin Anatomy
Who gets melanoma?
About 105,000 new skin melanomas are diagnosed in the U.S. every year, according to the National Cancer Institute. Roughly 1.5 million Americans are living with the condition.
Causes and risk factors
Sun exposure: Damage from repeated exposure to ultraviolet rays — from the sun or tanning beds — is a factor in roughly half of melanomas. Ultraviolet rays damage the skin’s DNA, which can lead to cancer.
Family and medical history: About half of melanoma cases are linked to an inherited genetic trait. If a close relative — a parent, sibling or child — has had melanoma, you are at a slightly higher risk. Also, if you’ve had melanoma or basal or squamous cell skin cancer, you are at higher risk. OHSU offers expert genetic counseling and testing to learn about your risk and how to manage it.
Region: Oregon is among the top third of states for melanoma cases. On average, about 1,000 people in Oregon are diagnosed with melanoma every year, according to the National Cancer Institute. That amounts to about 23.5 cases per 100,000 residents. Within Oregon, Clackamas and Columbia counties have the highest incidence, with about 30 cases per 100,000 residents.
Race/ethnicity: Melanoma can strike anyone. It is more common among white people. Those with fair skin and with red or blond hair or blue or green eyes are at increased risk. But although people of color are less likely to get melanoma, they are more likely to die from it, because of delays in detection and diagnosis.
Age: About three in four cases are diagnosed in people age 55 or older. At the same time, melanoma is one of the most common types of cancer among those ages 25 to 39.
Gender: Melanoma is more common in men, but that varies by age. For those younger than 50, women are at higher risk. For those older, men are.
Survival rates
The 5-year survival rate for melanoma is 94.7%. The rate is more than 99% for patients diagnosed before the cancer spreads.
This rate reflects the percentage of people, on average, who are alive 5 years after they were diagnosed compared with the general population.
It’s important to remember that these are averages. Your outlook will vary based on factors specific to you.
Melanoma symptoms
Most moles are normal and harmless. But if you notice a mole that seems different, talk to your doctor. It’s important to be familiar with your own skin so you recognize when something looks different.
You can also use the ABCDE guide:

A. Asymmetry: One side is not like the other.

B. Border: The edges are irregular or ragged.

C. Color: It has color variations, such as shades of brown or black, sometimes with patches of pink, red or white.

D. Diameter: It’s more than 6 millimeters across (the size of a pencil eraser), though it can be smaller.

E. Evolving: The mole may change in size, color or shape.
Other symptoms to watch for:
- A spot that stands out — one that's new or looks different from your other moles.
- A sore that doesn’t heal.
- Swelling or redness beyond the mole’s border.
- Itchiness, tenderness or pain at the mole.
- A mole that is scaly, that oozes or bleeds, or that includes a lump or bump.
Types
- Superficial spreading melanoma: This type makes up about 70% of cases. It's the most common type in young people. The first symptom is a flat or slightly raised discolored patch with irregular borders. The patch may be tan, brown, black, red, blue or white. It can be anywhere on the body, but it's most likely on the upper back, or on the torso in men and the legs in women. This melanoma grows on the top skin layer for quite a while before invading deeper tissue.
- Lentigo maligna: This type also stays close to the skin surface for a while. Most often, it appears flat or slightly elevated. It's most often tan, brown or dark brown. This type, which makes up about 10-15% of melanoma cases, is most often found in elderly people.
- Nodular melanoma: This type is often invasive by the time it is diagnosed. It often appears as a bump that’s usually black but sometimes brown, tan, red, white, blue or gray. It makes up 10-15% of melanoma cases and is the most aggressive type.
- Acral lentiginous melanoma: This type makes up 2-3% of melanoma cases. It usually appears as a black or brown discoloration under the fingernails or toenails, or on the palms or the soles of the feet. It's most often found in people with darker skin. It's the most common melanoma in Black people and Asian people.
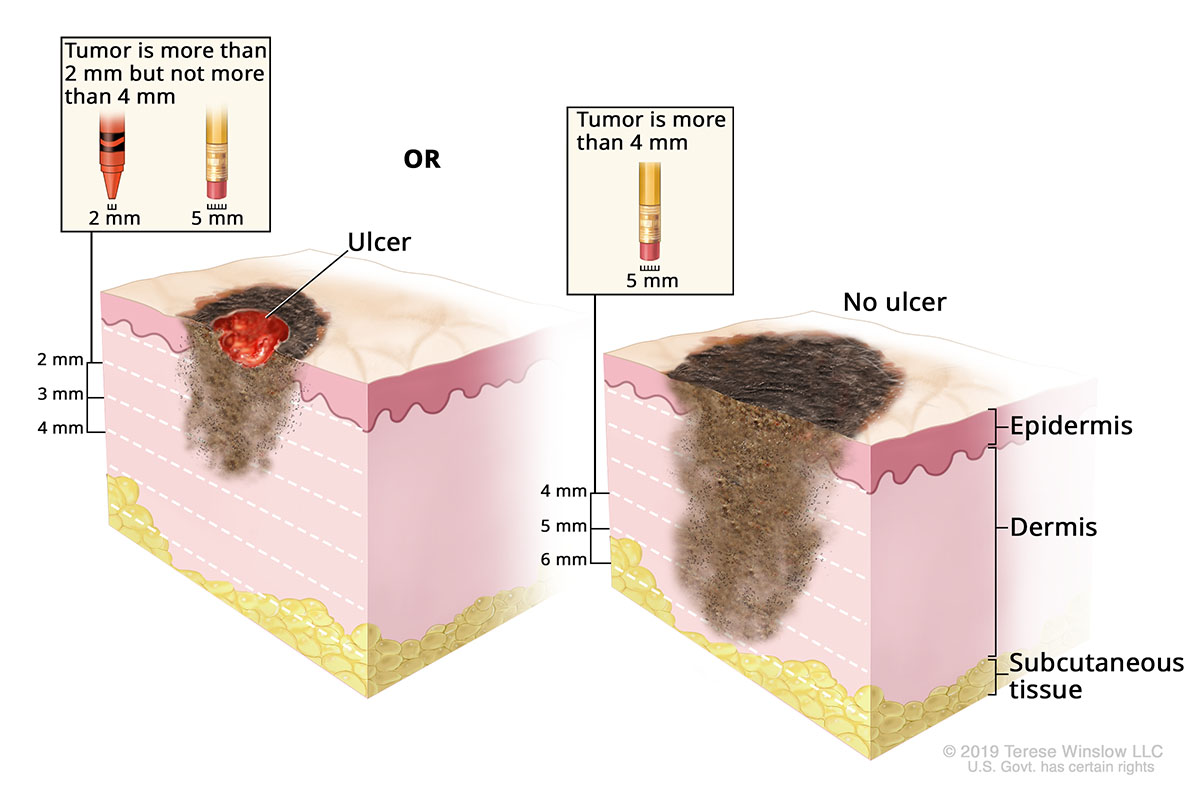
Stages of melanoma
Your treatment depends on the stage of your melanoma. Your care team will determine the stage based on:
- How deep the cancer is in your skin.
- Whether there's ulceration (an open sore).
- Whether cancer has spread to lymph nodes and/or other parts of your body.
Stage IIB Melanoma
- Stage I: The melanoma is less than 1 millimeter thick and is not found in the lymph nodes or other parts of the body.
- Stage IA: The melanoma is less than 0.8 millimeter thick and does not have ulceration.
- Stage IB: The cancer is less than 0.8 millimeter thick and has ulceration, or it's 0.8 to 1 millimeter thick and ulcerated or not.
- Stage II: The melanoma is thicker but not in the lymph nodes or other parts of the body.
- Stage IIA: The melanoma is thicker than 1 millimeter but no thicker than 2 millimeters and is ulcerated. Or it’s thicker than 2 millimeters but no thicker than 4 millimeters and not ulcerated.
- Stage IIB: The melanoma is thicker than 2 millimeters but no thicker than 4 millimeters and is ulcerated, or it's thicker than 4 millimeters and not ulcerated.
- Stage IIC: The melanoma is thicker than 4 millimeters and ulcerated.
- Stage III: Cancer may affect lymph nodes and/or nearby skin areas.
- Stage IIIA: The melanoma is less than 0.8 millimeters thick and may or may not be ulcerated, or it's up to 2 millimeters thick and not ulcerated. Cancer affects as many as three lymph nodes.
- Stage IIIB: One of the following:
- There's no sign of a primary tumor, but cancer affects one lymph node or has spread to nearby skin areas.
- The melanoma is less than 0.8 millimeter thick and may or may not be ulcerated, or it's up to 2 millimeters thick and not ulcerated. Cancer affects as many as three lymph nodes or affects nearby skin areas.
- The melanoma is up to 2 millimeters thick and is ulcerated, or it's up to 4 millimeters thick and not ulcerated. Cancer affects as many as three lymph nodes, or it affects nearby skin areas.
- Stage IIIC: One of the following:
- There's no sign of a primary tumor. Cancer may affect up to four or more lymph nodes; matted (connected) nodes may be present; and cancer may have spread to nearby skin areas.
- The melanoma is less than 0.8 millimeter thick and may or may not be ulcerated, or it's up to 4 millimeters thick and is not ulcerated. Cancer may affect up to four or more lymph nodes; matted nodes may be present; and cancer may have spread to nearby skin areas.
- The melanoma is more than 2 millimeters thick but no more than 4 millimeters thick and is ulcerated, or it's thicker than 4 millimeters and not ulcerated. Up to one lymph node is affected, or cancer affects nearby skin areas.
- The melanoma is thicker than 4 millimeters and ulcerated. Cancer affects up to one lymph node and nearby skin areas, or it affects as many as three nodes and no nearby skin areas.
- Stage IIID: The melanoma is thicker than 4 millimeters and ulcerated. Cancer may affect as many as four or more lymph nodes; matted nodes may be present; and cancer may have spread to nearby skin areas.
- Stage IV: The melanoma has spread to organs such as the lungs, liver or brain.
Genetic testing for melanoma
Learn more
War on Melanoma
The War on Melanoma is an all-fronts effort to eliminate melanoma in Oregon. Resources include:
- Educación Sobre el Melanoma
- For the public: Melanoma Early Detection interactive learning tool
- For health care professionals: Melanoma Early Detection Toolkit
- For skin-aware professionals: Skin Crew
- Melanoma Community Registry
- Mole Mapper smartphone app
- Start Seeing Melanoma public health campaign
More on melanoma
- Melanoma Skin Cancer, American Cancer Society
- Melanoma Overview, Skin Cancer Foundation
- Skin Cancer: Everyone's at Risk, American Academy of Dermatology
- Skin Cancer (Including Melanoma), National Cancer Institute
Location
Knight Cancer Institute, South Waterfront
Center for Health & Healing, Building 2, ninth floor
3485 S. Bond Ave.
Portland, OR 97239
Free parking for patients and visitors
Cancer clinical trials
Clinical trials allow patients to try a new test or treatment.
See melanoma
By checking your own skin, you could save your own life. Learn what to look for and what to do if you find something. Start seeing melanoma.
Read more
Learn more about OHSU Knight Cancer Institute treatments: