Endometrial Cancer (Uterine Cancer)

There are two primary kinds of uterine cancers, endometrial cancer and uterine sarcoma. This page discusses endometrial cancer. Visit our uterine sarcoma page.
Endometrial cancer is also called uterine cancer. It develops in the endometrium, the lining of the uterus. The uterus is where a baby grows during pregnancy.
Endometrial cancer can be hard to find, but it’s highly treatable when found early.
The OHSU Knight Cancer Institute is known for sensitive cancer care. You’ll find:
- Expert diagnostic imaging, with fast results
- Advanced genetic testing to guide your care
- The latest treatments, including clinical trials and targeted therapies
- Nurses who guide you through your care
- Support services, including help for fertility after cancer
What is endometrial cancer?
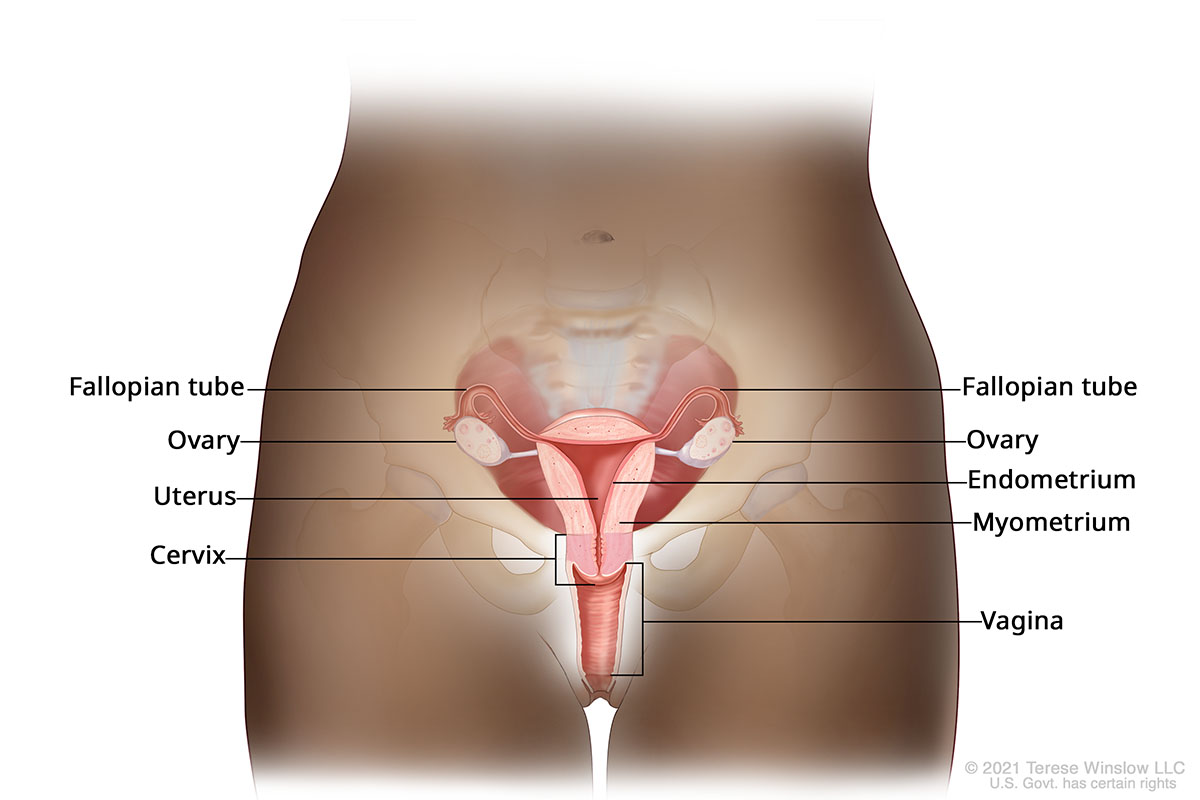
Anatomy of the female reproductive system
What is endometrial cancer?
Endometrial cancer is a type of uterine cancer. It arises in the endometrium, the lining of the uterus, the small, pear-shaped organ inside the pelvis. Sometimes cells in the endometrium start to divide and multiply out of control, forming tumors.
Endometrial cancer starts in the uterus, a hollow pear-shaped organ in the pelvis. The uterus has a lining called the endometrium. Sometimes cells in the endometrium start to grow out of control, leading to cancer.
Types of endometrial cancer
Endometrioid adenocarcinoma: This is the most common type, making up about 75% of cases. It is usually found early, often because of abnormal bleeding. It tends to grow slowly. Sometimes it can be treated with just surgery.
Serous adenocarcinoma: This makes up about 10% of cases. It is usually found in older women who are past menopause. It tends to grow quickly and is more likely to spread outside the uterus.
Clear cell carcinoma: This is a rare type. It can spread early and often needs more aggressive treatment.
Carcinosarcoma: This type is more likely to spread and often needs aggressive treatment.
Who gets endometrial cancer?
Endometrial cancer is the most common female reproductive cancer in the U.S. About 69,000 cases are diagnosed each year. About 886,000 people are living with endometrial cancer in the U.S.
Risk factors
Anyone with a uterus is at some risk. Risk factors are often tied to higher exposure to estrogen.
Hormone-related risks:
- High estrogen without progesterone: Taking estrogen replacement therapy without progesterone after menopause increases risk.
- Tamoxifen: Taking this drug to prevent and treat breast cancer can slightly increase risk.
Medical conditions:
- High body fat: Fat tissue can make estrogen, raising estrogen levels in the body.
- Polycystic ovary syndrome (PCOS): People with this condition don’t have regular periods. That keeps estrogen levels high.
- Endometrial hyperplasia: This happens when the lining of the uterus thickens.
Reproductive and menstrual history:
- Early menstruation or late menopause: More years of menstruation mean longer exposure to estrogen.
- Never having been pregnant: This means more menstrual cycles, which can raise risk.
Age and family history:
- Being older: Risk rises after menopause.
- Family history: Having a close blood relative with endometrial cancer raises risk. Inherited conditions such as Lynch syndrome can greatly raise risk. We provide genetic counseling and testing.
Survival rates
The five-year relative survival rate for endometrial cancer is 81%. This is the portion of people who are alive five years after diagnosis compared with the general population. The rate rises to 95% if the cancer is found before it spreads.
It's important to remember that survival rates are averages. They can't predict any one person’s outcome.
Endometrial cancer signs and symptoms
Endometrial cancer is often found early because it causes symptoms.
If you have gone through menopause, tell your doctor right away if you have vaginal bleeding or spotting, or discharge that is unusual.
If you have not gone through menopause, tell your doctor about any of these symptoms:
- Bleeding between periods
- Very heavy or long periods
- Bleeding after sex
Other symptoms can include:
- Pain during sex or when peeing
- Weight loss without trying
These symptoms may have other causes. It’s best to tell your doctor if you have these symptoms so you can get the right care.
Endometrial cancer diagnosis
There is no standard screening test for endometrial cancer. If your doctor thinks you may have endometrial cancer, you may have one or more of these tests:
Ultrasound: This uses sound waves to create an image of the uterus. A small device is placed in the vagina to give your doctor a better look at the uterus.
Hysteroscopy: This uses a thin, flexible tube with a camera inside to look inside the uterus. Your doctor may collect tissue samples.
Biopsy: Your doctor uses a thin tube to take a bit of tissue from the endometrium to be looked at under a microscope.
Dilation and curettage: This test is also called a D&C. If biopsy results are unclear, your doctor may take a larger tissue sample. This is done by gently opening the cervix and taking tissue from the uterus.
Genetic testing: Your doctor may recommend testing for inherited genetic changes. Results can help your team plan treatment. Your team may also analyze your cancer’s genetic makeup to match you with the most effective treatments.
Endometrial cancer stages
Doctors use stages to describe how much cancer is in the body and how much it has spread.
Endometrial cancer stages go from stage I to stage IV (4). A higher number indicates more spread. Staging is complex and varies from person to person. It’s best to talk with your doctor about your stage.
Stage I: The cancer is only in the uterus. If it’s a slower-growing type, it may also be in an ovary.
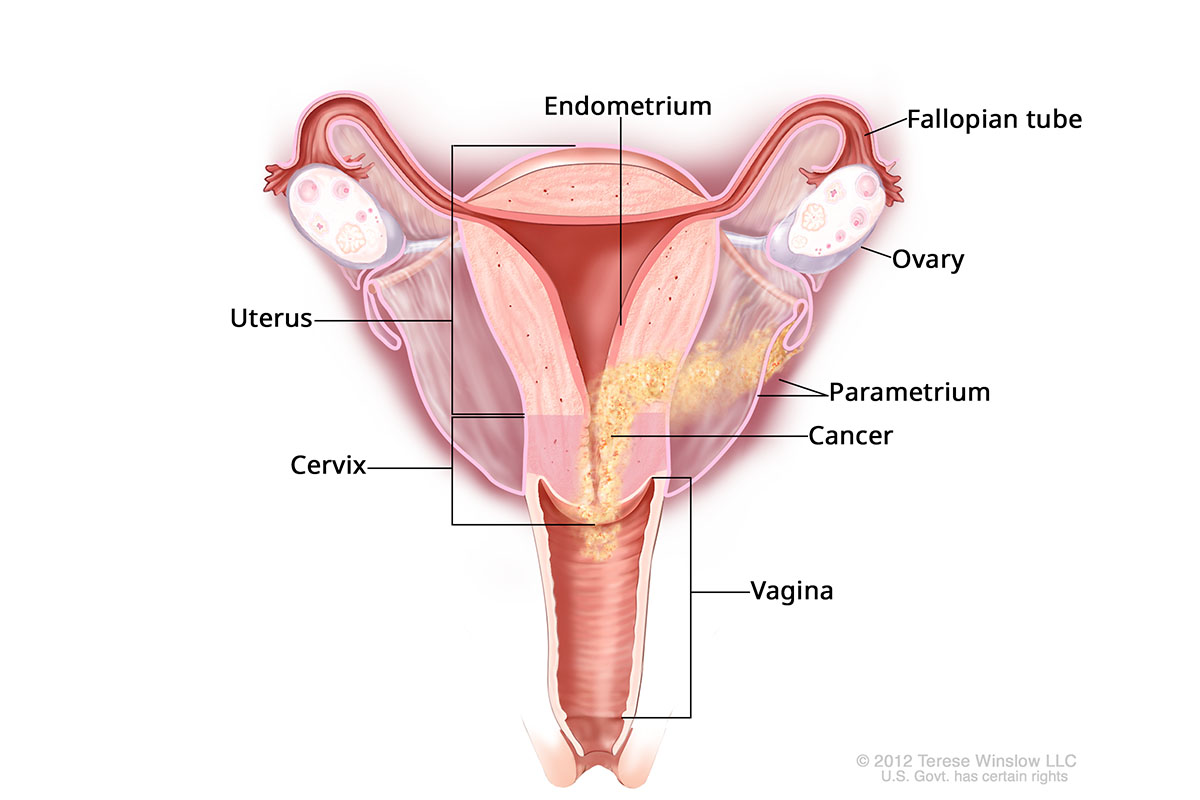
Stage II: The cancer may have spread to the cervix or blood or lymph vessels. It may be in the uterus’ middle layer (myometrium).
Stage III: The cancer has spread outside the uterus.
Stage IV: The cancer may have spread to the rectum, bladder or abdomen lining or outside the abdomen.
Stage IIIB Endometrial Cancer
Grade
Endometrial cancer may also be described by its grade, from G1 to G3. Grades are based on how much cancer cells look like healthy cells under a microscope. The more different they look, the higher the grade, and the more likely the cancer is to spread.
Endometrial cancer treatment
Your care team will work with you to tailor a plan to your diagnosis, health and desire to have children.
Surgery
Surgery is often recommended to remove as much of the cancer as possible. We use robotic surgery for less pain, less time in the hospital and quicker recovery.
Surgery for endometrial cancer often means removing the uterus. This is called a hysterectomy.
In most cases, the fallopian tubes and ovaries are also removed to lower the chance of cancer coming back. This procedure is called a bilateral salpingo-oophorectomy.
At OHSU, we also check during surgery for cancer in your lymph nodes. These are small glands that act like filters in fighting infection. They can trap cancer cells, giving doctors one way to see if the cancer has spread.
We use a technique called sentinel lymph node mapping. Your doctor injects a bit of dye into the uterus. This dye goes to the first lymph nodes that drain the uterus. These nodes are removed and looked at under a microscope to check for cancer cells. The results help your care team decide whether other treatments are needed.
Radiation therapy
Radiation therapy uses beams of energy to stop cancer cells from growing. At OHSU, we have radiation oncologists who focus on treating endometrial cancer. Options include:
- External beam radiation: This uses a machine outside the body to target the cancer.
- Brachytherapy: This uses a small device or temporary implant to deliver radiation inside the body. The device or implant is placed near the site of the cancer.
Chemotherapy
Chemotherapy drugs are used to kill or stop the growth of cancer cells. The drugs are usually given in a series of IV drips called infusions. You may get one drug or a mix of drugs. Chemotherapy is most often used after surgery to lower the risk of the cancer coming back. Chemotherapy can also help ease symptoms in advanced cancer.
Hormone therapy
Hormones are chemical messengers in the body. They include estrogen, a female sex hormone.
Some endometrial cancers grow when hormones like estrogen attach to the cancer cells. Hormone therapy can be used to block these hormones or lower their levels when:
- The cancer has come back after surgery
- The cancer has spread past the uterus
- Surgery or radiation therapy are not safe to use
- A patient wants to have children
Hormone therapy may be given as a pill, liquid or shot.
Targeted therapy
Targeted therapy drugs lock onto cancer cells and shut them down, leaving healthy cells mostly unharmed.
Targeted therapy is used most often:
- For endometrial cancer that has come back or spread
- When chemotherapy won’t work
Targeted therapy drugs are usually given as pills or by IV. They may be combined with other treatments, such as immunotherapy.
Immunotherapy
Immunotherapy drugs help immune cells find and kill cancer cells. The most common immunotherapy drugs are called checkpoint inhibitors. They help immune cells better recognize and attack cancer cells.
Fertility-sparing treatment
In some cases we may use a treatment that spares the uterus and ovaries. This treatment is used only if:
- The cancer has not spread past the uterus
- The cancer does not seem aggressive
- The patient has a strong desire to stay fertile
Fertility-sparing treatment most often uses hormone therapy. This needs close watching to make sure the cancer is responding.
If you are able to use this treatment, you’ll have access to our fertility specialists.
Learn more
- Endometrial Cancer, American Cancer Society
- Uterine/Endometrial Cancer/GTD, Foundation for Women’s Cancer
Endometrial cancer team
Gynecologic oncologists
-
- Amanda Bruegl, M.D. (she/her)
- Accepting new patients
-
- Amanda J. Compadre, M.D. (she/her/ella)
- Accepting new patients
-
- Ross Harrison, M.D., M.P.H. (he/him)
- Accepting new patients
-
- Breana L. Hill, M.D. (she/her)
- Accepting new patients
-
- Jessica Jou, M.D., M.S., FACOG (she/her)
- Accepting new patients
-
- Elizabeth Munro, M.D.
- Accepting new patients
Radiation oncologists
-
- Cheryl Claunch, M.D., Ph.D. (she/her)
- Accepting new patients
-
- Casey Williamson, M.D., M.A.S. (he/him)
- Accepting new patients
Location
Knight Cancer Institute, South Waterfront
Center for Health & Healing, Building 2
3485 S. Bond Ave.
Portland, OR 97239
Free parking for patients and visitors
Refer a patient
- Refer your patient to OHSU.
- Call 503-494-4567 to seek provider-to-provider advice.
Cancer clinical trials
Clinical trials allow patients to try a new test or treatment.
Read more
Learn more about OHSU Knight Cancer Institute treatments:
Stay informed
News: Read about research breakthroughs, patient care and many other topics on our OHSU News site.