Liver Cancer

Liver cancer happens when cancer cells form in the liver. Cancer can also spread to the liver from another part of the body.
The National Cancer Institute recognizes the OHSU Knight Cancer Institute as one of the best places in the nation to receive cancer care.
At the Knight, you will find:
- World-class experts in cancers of the digestive system
- The only liver transplant center in Oregon
- One of the few Northwest hospitals with hepatic arterial infusion, an advanced therapy
- A team of specialists working together
- Nurses who guide you through treatment
- Social workers, dietitians and other cancer experts to support you
- Hundreds of clinical trials
Quick links
What makes us different
Highly trained teams: Our doctors have advanced training in areas such as liver transplant surgery. They can treat the most complex cases.
Nurse navigators: Our experienced nurses guide you through treatment so you can focus on your well-being. They can arrange appointments, answer questions and coordinate care across providers.
Innovation: The Knight is a leader in radiation therapy to target cancer while avoiding healthy tissue.
National excellence: We are research leaders. Our Cancer Early Detection Advanced Research Center, or CEDAR, focuses on finding cancer early. Our teams also work to quickly turn lab discoveries into treatments.
Teamwork: We are the only program in Oregon where specialists meet weekly to develop treatment recommendations patient by patient. Your team might include:
- Hepatologists, who specialize in diagnosing and treating all types of liver disease
- Transplant surgeons who are part of our decades-long program
- Cancer doctors who specialize in a range of treatments, from surgery to targeted therapy
What is liver cancer?
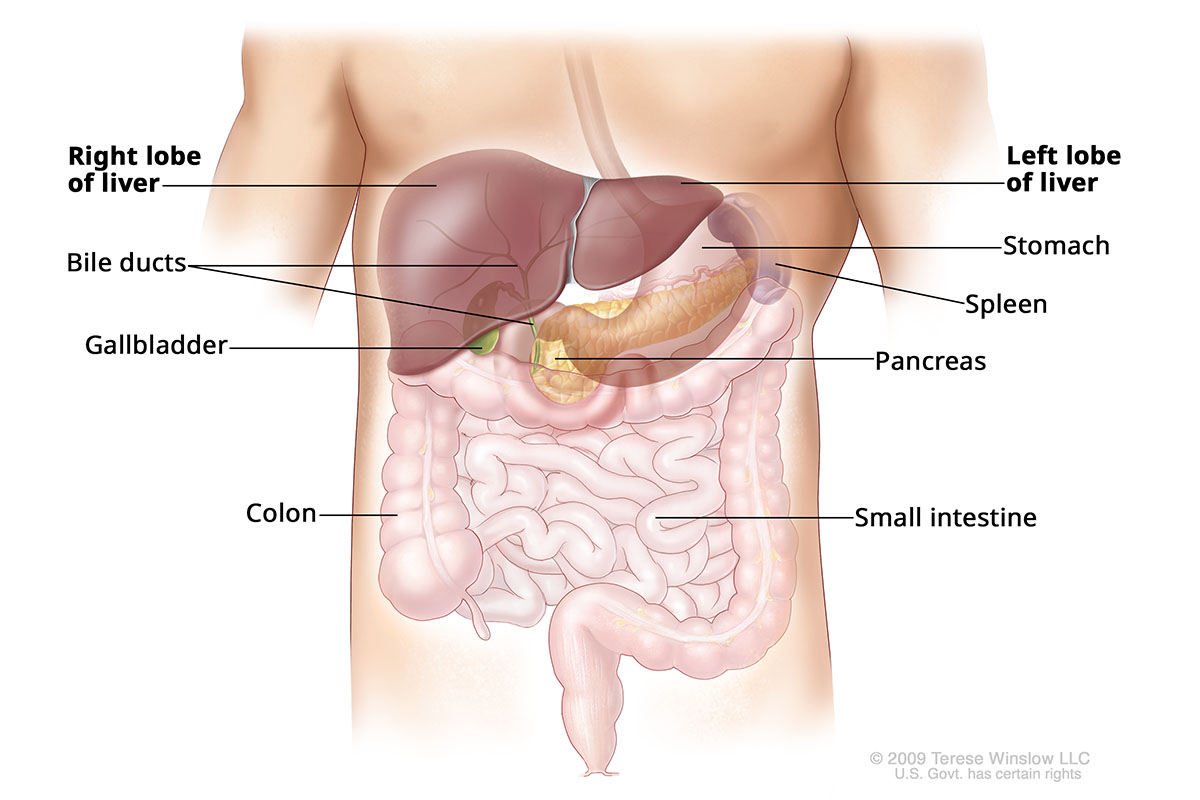
The liver is a football-shaped organ that helps the body digest fat and store sugar. It is one of the body's largest organs. The liver also filters toxins and other substances, such as alcohol or drugs, from the blood. Cancer that starts in the liver happens when liver cells grow out of control.
Liver Anatomy
Types of liver cancer
Liver cancer that starts in the liver is also known as primary liver cancer. It has several subtypes:
- Hepatocellular carcinoma: HCC is the most common cancer that starts in the liver. It grows in cells that make up 80 percent of the liver.
- Intrahepatic cholangiocarcinoma: ICC, also known as bile duct cancer, grows in cells lining the bile ducts that run through the liver.
- Angiosarcoma and hemangiosarcoma: These fast-growing types are rare. They develop in cells lining the liver’s blood vessels.
Cancer can also start in another part of the body and spread to the liver. In the U.S., this type is more common than cancer that starts in the liver.
Cancer that spreads from elsewhere in the body is treated differently. For example, colon cancer that spreads to the liver is called colon cancer with liver metastasis or metastatic colon cancer. It is treated like colon cancer.
Who gets liver cancer?
About 42,000 people are diagnosed with primary liver and bile duct cancer in the U.S. each year, according to the National Cancer Institute.
Learn about liver cancer risk factors.
Liver cancer survival rates
Early detection is important. More than half of patients with small, removable tumors and no other serious condition live at least five years after diagnosis with liver cancer. Outcomes are more discouraging if the cancer is found after it has spread.
It’s important to remember that survival rates are averages. They can’t predict what will happen to you.
Signs of hope: The five-year survival rate for liver cancer has steadily improved since 2000. Researchers at the Knight Cancer Institute are working on new ways to treat liver cancer. Your care team can help you decide if you might benefit from a clinical trial.
Quality of life: While liver cancer sometimes cannot be cured, treatment can keep you comfortable and give you time to do things you enjoy. Your Knight Cancer Institute team will strive to give you the longest, highest-quality life possible.
Clinical trials and research
The Knight is a leader in clinical trials. These are research studies that test new treatments and approaches in humans. We are known worldwide for cancer research, including targeted therapies that precisely attack liver cancer. Our cancer registries, including one for liver tumors, help researchers better understand cancer. Patients who take part gain access to updates.
Learn more
- Liver and Bile Duct Cancer, National Cancer Institute
- Liver Cancer, American Cancer Society
Location
Knight Cancer Institute, South Waterfront
Center for Health & Healing, Building 2
3485 S. Bond Ave.
Portland, OR 97239
Free parking for patients and visitors
Refer a patient
- Refer your patient to OHSU.
- Call 503-494-4567 to seek provider-to-provider advice.
Cancer clinical trials
Clinical trials allow patients to try a new test or treatment.
Read more
Learn more about OHSU Knight Cancer Institute treatments:
Stay informed
News: Read about research breakthroughs, patient care and many other topics on our OHSU News site.