Myeloma

The OHSU Knight Cancer Institute provides expert care for multiple myeloma and other plasma cell disorders. Our doctors focus on specific blood disorders, giving them rare expertise on the best treatments for your condition. Our care and treatment options include:
- A range of specialists working together to develop the most effective treatment recommendations for you.
- A weekly meeting where doctors from multiple specialties combine their expertise to tailor care to your needs.
- Expertise in rare plasma cell disorders, such as POEMS syndrome, light chain deposition disease, and AL amyloidosis.
- A nurse coordinator who can arrange your appointments and answer your questions.
- Oregon’s largest bone marrow/stem cell transplant program.
- A type of immunotherapy called CAR T-cell therapy for multiple myeloma.
- Access to promising new treatments through clinical trials led by some of the world’s leading blood cancer researchers.
- Support services to help you and your family manage cancer treatment and side effects.
Understanding multiple myeloma
What is multiple myeloma?
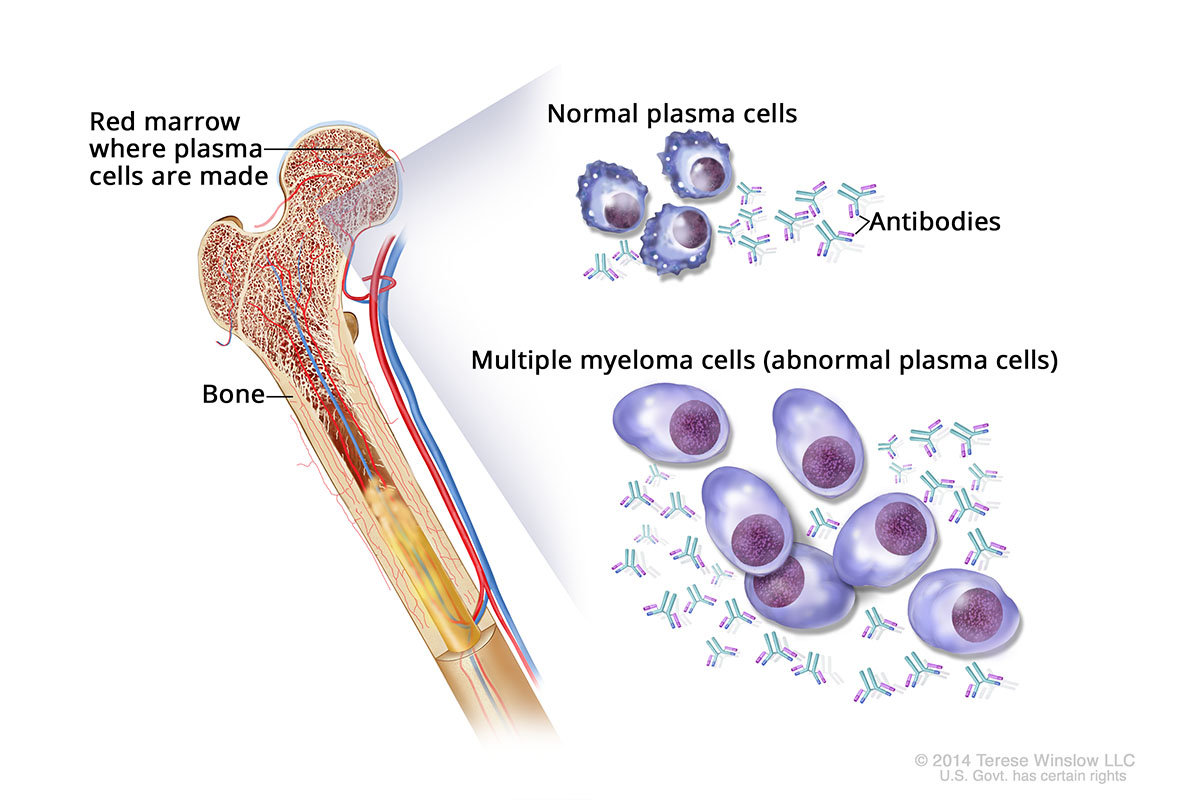
Multiple myeloma is a cancer of the plasma cells, a type of blood cell found in bone marrow. These cells normally make antibodies that kill germs. When the plasma cells grow out of control, they can crowd out normal cells in the bone marrow, form tumors and release abnormal proteins. Eventually, these changes can damage organs or bones, and lead to infections.
Patients with myeloma are classified as having either:
- Asymptomatic (smoldering) myeloma: These patients don't have symptoms and, outside of clinical trials to test therapies, don't receive treatment.
- Active (symptomatic) myeloma: These patients have symptoms and receive treatment.
Multiple Myeloma
Who gets multiple myeloma?
About 36,000 new cases of multiple myeloma are diagnosed in the U.S. every year, according to the National Cancer Institute. Roughly 192,000 people in the U.S. are living with the disease.
The cause is unknown, but risk factors include:
- Age: More than 85% of patients are 55 or older at diagnosis.
- Race: Black people are at higher risk.
- Family history: Having a parent, child or sibling with the disease is linked to higher risk for reasons scientists don’t fully understand.
Survival rates for multiple myeloma
A key concept in understanding survival is five-year relative survival rate. This is the percentage of people who are still alive five years after they were first diagnosed, compared to the general population. (It doesn’t count death from other causes.)
Survival rates for multiple myeloma are better if the condition is caught early. Unfortunately, the condition is often not caught until it has spread.
The overall five-year relative survival rate for multiple myeloma is 62%, according to the National Cancer Institute. The rate is 80% for people whose myeloma is caught before it spreads.
It's important to remember that statistics are averages and can’t predict the outcome for any one patient. It's also important to remember that these figures are based on the treatments that were available more than five years ago. Patients who are diagnosed now may have a better outlook. Treatments are getting better all the time. Over the last 30 years, for example, the survival rate for multiple myeloma has doubled.
Symptoms of multiple myeloma
You may not have symptoms early on. When you do have symptoms, they can include:
- Bone pain
- Nausea and appetite loss
- Weight loss
- Confusion
- Frequent, severe infections
- Numbness or weakness in legs
Diagnosing multiple myeloma
A routine blood test, physical exam and medical history are often the first steps in making a diagnosis. Additional tests may include:
Blood and urine tests: Doctors use these tests to measure blood protein levels and to see how aggressive the cancer is.
Imaging tests: Scans can look for bone damage caused by multiple myeloma.
Bone marrow biopsy: We collect tissue and fluid from your bone marrow with a thin needle. Doctors examine the samples to look for plasma cells and abnormal proteins.
Multiple myeloma stages
Doctors assign a stage to your myeloma to indicate how advanced it is and what kind of treatments will work best. We use a staging system that looks at:
- Levels of two proteins, albumin and beta-2-microglobulin
- The amount of a substance called lactate dehydrogenase, or LDH, in your blood
- Genetic abnormalities
Stage I: Beta-2-microglobulin is less than 3.5 milligrams per liter. The albumin level is at least 3.5 grams per deciliter. LDH levels are normal. No “high-risk” genetic abnormalities are found.
Stage II: Not Stage I or III.
Stage III: Beta-2-microglobulin is at least 5.5 milligrams per liter. LDH levels are high. “High-risk” genetic abnormalities are present.
Multiple myeloma treatments

The Knight Cancer Institute takes a team approach to your care. A nurse coordinator will guide you through treatment and set appointments. Your care team will also include doctors and nurses who are experts in blood cancer. Other specialists will join your team based on your specific needs.
Team members gather each week in a meeting called a tumor board to go over treatment options as a group. This approach ensures that you benefit from the entire team’s knowledge. In addition to your hematologist-oncologist (blood and cancer expert), specialists may include:
- Cardiologists (heart doctors)
- Nephrologists (kidney doctors)
- Gastroenterologists (digestive system doctors)
- Neurologists (brain, spinal cord and nerve doctors)
- Interventional radiologists (doctors who do image-guided procedures)
- Orthopaedic (bone) surgeons
Though multiple myeloma does not have a cure, treatments can make it manageable over time. Patients with asymptomatic disease (no symptoms) may live years without needing treatment. When treatment is needed, options include the following, alone or in combination:
Chemotherapy: Single or combined medications are given by mouth or injected under the skin or into a vein. They circulate in the bloodstream to kill cancer cells. To improve effectiveness, chemotherapy may be used in combination with other medications, such as steroids.
Immunotherapy: Immunotherapy medications help the immune system weaken or destroy cancer cells. Among other research innovations, OHSU took part in studies that led the Food and Drug Administration to approve the immunotherapy medication Darzalex (daratumumab) to treat multiple myeloma.
CAR T-cell therapy: The FDA approved Abecma to treat people 18 and older with multiple myeloma that did not respond, or that returned, after four other therapies. CAR T-cell therapy is a gene therapy and a type of immunotherapy. T cells (infection-fighting immune cells) are collected from the patient's blood, genetically modified to fight cancer, then returned to the patient in an IV drip.
Targeted therapy: These medications target abnormal cells at the molecular level, limiting damage to normal ones. Depending on the medication, this therapy is given in a shot, IV or pill.
Radiation therapy: This treatment uses beams of radiation to destroy abnormal cells. For multiple myeloma, we primarily use external beam radiation. A machine outside the body delivers radiation to kill cancer cells. OHSU was the first center in Oregon to use image-guided radiation therapy to precisely target cancer cells while sparing healthy tissue.
Bone marrow/stem cell transplant: Diseased cells are destroyed with chemotherapy and radiation, then replaced with transplanted healthy cells. The new cells rebuild your immune system to help you fight infection and disease. OHSU has the largest transplant center in Oregon.
Other therapies for multiple myeloma
These therapies may help manage symptoms and side effects of treatment.
Bone therapies: Myeloma cells can dissolve or weaken bones. Bisphosphonates are IV medications that can counteract the damage and prevent further bone loss. Denosumab, a type of immunotherapy given in a shot, targets cells that weaken bone.
Kyphoplasty and vertebroplasty: Myeloma can cause bone fractures in your spine. Minimally invasive kyphoplasty and vertebroplasty inject plastic cement into the spinal column to stabilize your spine and reduce pain.
Complementary medicine: We offer acupuncture and other complementary therapies to ease the side effects of treatment for multiple myeloma.
Multiple myeloma clinical trials and research
Clinical trials: We offer access to leading-edge clinical trials for patients with all stages of multiple myeloma. Our doctors work with researchers nationwide to develop new treatments for myeloma patients, including those who no longer benefit from standard therapies.
Cancer registries: Cancer registries are databases of patient information that can include blood and tissue samples. They help scientists understand how cancer works so they can develop better treatments and work toward cures. Learn about our registries, including one for bone marrow transplant patients, and see how you can contribute to research.
Learn more
- Multiple Myeloma, American Cancer Society
- Understanding Multiple Myeloma, Multiple Myeloma Research Foundation
- Plasma Cell Neoplasms (Including Multiple Myeloma), National Cancer Institute
Locations
Knight Cancer Institute, South Waterfront
Center for Health & Healing, Building 2
3485 S. Bond Avenue
Portland, OR 97239
Free parking for patients and visitors
Refer a patient
- Refer your patient to OHSU.
- Call 503-494-4567 to seek provider-to-provider advice.
Cancer clinical trials
Clinical trials allow patients to try a new test or treatment.
Read more
Learn more about OHSU Knight Cancer Institute treatments:
Stay informed
News: Read about research breakthroughs, patient care and many other topics on our OHSU News site.