Pediatric Critical Care Medicine Fellowship

Message from the program director

Welcome to the Pediatric Critical Care Medicine Fellowship Program at Oregon Health & Science University (OHSU)/Doernbecher Children’s Hospital in Portland. We are excited that you are considering us for your fellowship training!
Our fellowship was born in 2011, when a core group of academic and clinical faculty recognized that the OHSU PICU offered incredible training opportunities. Our busy medium-size PICU offers a wide variety of cases cared for by a cadre of highly-skilled intensivists who are excited to train the next generation.
We are a great fit for pediatricians who are passionate clinicians. We seek applicants with vision and drive to thrive in a flexible, individualized program. Our program is ideal for candidates who desire clinical rigor with time to nurture specific professional interests. Please review our program aims below to learn more about what makes Doernbecher a special place to train.
Our program is small, but mighty; with one fellow in each of three years of training, we are able to tailor our curriculum to meet individual needs and career goals. Our fellows work alongside faculty more as colleagues than as trainees. Our tight-knit group of faculty members is uniquely positioned to guide each fellow as they develop into independent, confident, and compassionate pediatric intensivists. An emphasis on faculty mentorship – personal and professional – inspires fellows to join them in scholarly activities related to quality improvement, patient safety, and clinical research.
Since 2015 we have graduated an outstanding pediatric intensivist every year, all of whom have gone on to great careers. Our ABP Critical Care Board Exam pass rate is 100%. More importantly, our graduating fellows excel in the management of critically ill children with multisystem disease. Each has their own professional niche and expertise.
Our current fellows are each making integral contributions toward the research, educational, service, and clinical missions of the institution – as we speak! They are recognized throughout the pediatric community for their teamwork with clinical staff, residents, other fellows, and faculty.
We do this in the setting of beautiful Portland, Oregon. Our fellows work hard, play hard, and finish training well positioned and well balanced to enter the next phase of their career. We hope this website will give you a glimpse into our fellowship program and PICU family, our city, and details about our interview day. Please let us know if you have any questions regarding our training program. We hope to meet you soon!
With gratitude,
Erin C. Burns, M.D.
Fellowship Program Director
Program aims
The Pediatric Critical Care Medicine Fellowship is a three-year subspecialty training program designed to follow residency training in pediatrics or combined internal medicine-pediatrics, though non-traditional routes are possible as well. The fellowship program seeks to develop outstanding clinicians, educators, researchers, and leaders in pediatric critical care medicine. With one fellow per training level, we are a small program with the ability to prioritize educational goals. Curricula will vary as they are tailored to individual fellow circumstances, career goals, American Board of Pediatrics approval, and other needs.
OHSU is where healing, teaching, and discovery come together. As Oregon’s only academic health center and medical school, we provide comprehensive healthcare, educate the next generation of pediatric intensivists, and explore new solutions to healthcare problems.
The Pediatric Critical Care Fellowship at Doernbecher Children’s Hospital trains academic physicians with an emphasis on provision of excellent patient care. We specifically focus on training compassionate and collegial physicians with strong communication skills and who work well in interdisciplinary teams. Given the multidisciplinary nature of critical care, strong teamwork is at the core of what we do and teach.
We have a diverse patient population providing breadth to the training of our fellows. In addition to our very experienced PICU faculty, we have an exceptional and comprehensive team of pediatric subspecialists to support the care of these patients and who are involved in the training of our fellows. Our graduating fellows excel in the management of critically ill children with multisystem disease.
With a PICU serving Oregon, southern Washington, eastern Idaho, and northern California, the fellows are exposed to a broad range of patients from rural and urban settings. They become adept in managing the complex transport of patients over long distances, using various modes of transport. Fellows will accompany our dedicated pediatric critical care transport PANDA Team on a select subset of transports longitudinally throughout training, with roles commensurate with their advancing skill levels. Another crucial aspect of care across long distances is the use of telemedicine. OHSU is home to one of the largest, most comprehensive telehealth networks in the world, and PICU fellows receive training in this important outreach modality.
We strive to develop fellows who are aware of the physical, cognitive, psychological, and social impact critical care admission has on patients and families in both the short and long term encompassed by the post-intensive care syndrome. Fellows participate in our critical care and neurotrauma recovery program through both inpatient consultation and outpatient follow-up. This is the only program of its kind on the West Coast. Fellows are educated in identification and management of post-intensive care syndrome through a multidisciplinary team that includes faculty in Pediatric Critical Care, Neurology, and Neuropsychology. Fellows will experience first-hand the range of recovery seen in patients surviving critical illness and acquired brain injury.
We believe that hard work today can result in a better tomorrow. To that end, fellows are trained in Quality Improvement (QI) science and methodology. Fellows participate in one or more team-based interdisciplinary projects aimed at improving patient care and safety, and over time develop skills to design, implement, and lead these projects independently.
We do this in the setting of beautiful Portland, Oregon, in a small but comprehensive program where fellows get to interact closely with faculty and are treated as individuals and colleagues. We feel this provides an optimal learning environment.
Benefits
Please see the Department of Pediatrics fellowship page for departmental benefits available to all pediatric fellows, and the OHSU GME page for Employment and Benefits information, including salary, transportation, and insurance.
Curriculum
Clinical training
The Doernbecher PICU is a 20-bed unit with an average daily census of 15 patients. We are an open, mixed unit with approximately 1400 admissions annually. Our diverse patient population includes pediatric medical, general surgical, cardiac medical and surgical, neurosurgical, renal transplant, and multi-system trauma patients. We care for approximately 13 ECMO cases per year, in addition to 150 patients who are status-post intra-operative cardiopulmonary bypass procedures.
Our catchment area includes Oregon, southern Washington, northern California, and Idaho. Doernbecher has an active and dedicated pediatric critical care transport team providing high-quality mobile ICU care to all of these regions, allowing PICU fellows to become facile and comfortable with management of pediatric transports (~1000 per year).

During 3 years of training, fellows develop skills critical to the management of the intensive care unit, including patient triage, leadership of a large team of medical trainees, cooperation with nursing leadership, and ongoing process improvement. Work hours during these clinical weeks consists of both day and night shifts. There are no 24 hour shifts, and no home call.
Sample Block Schedule
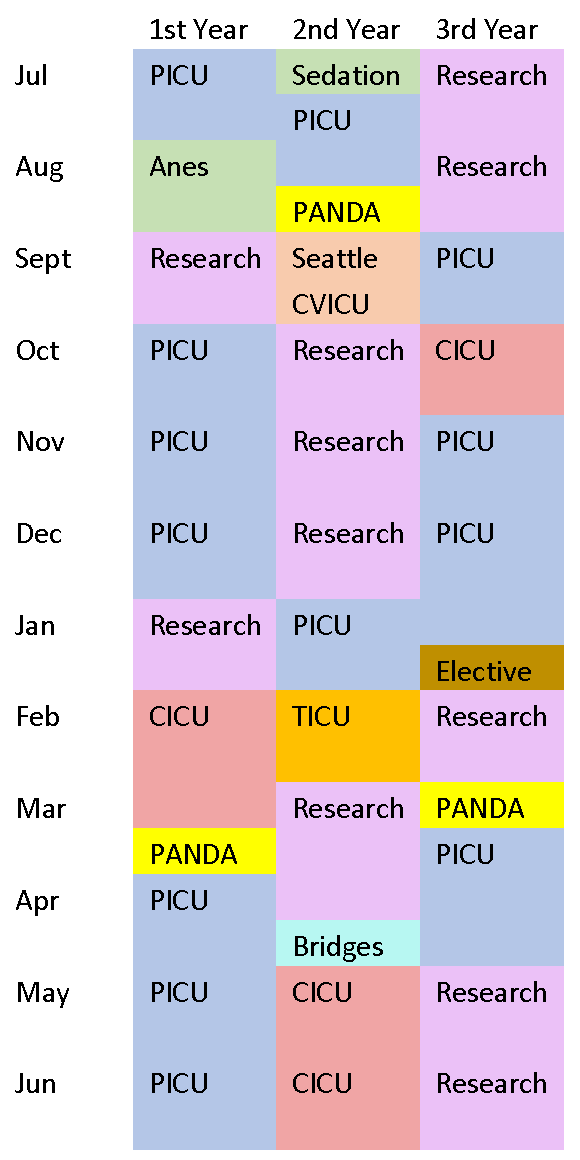
Notes:
Vacation time = 4 weeks/year + 1 week protected CME
PANDA = Pediatric and Neonatal Doernbecher Critical Care Transport Team
CICU = DCH Cardiac ICU Service
Seattle CVICU = 4 week rotation at Seattle Children's Hospital (optional)
TICU = OHSU Adult Trauma ICU
Our faculty are 14 Board-Certified Pediatric Intensivists, including 2 double-boarded Cardiac Intensivists, a team of PICU Advanced Practice Practitioners and a PICU Hospitalist. Attendings are in-house 24-7. Doernbecher is also home to a complete spectrum of pediatric subspecialty consultants with national and international reputations. With one fellow per year, there is always time for teaching!
Didactics
We believe that fellowship is a special, once-in-a-career opportunity to soak up knowledge and skills. As such, fellows’ education is always a priority, whether at the bedside or in the classroom.
Our didactic curriculum is designed to optimize the fellows’ ability to learn in a protected and meaningful way, while minimizing disruption to clinical and research duties. Protected educational time we call “Learning Lunes,” as it occurs each Monday afternoon for 1-3 hours. Comprising these hours are a rotating series of Core Physiology, PICU topical lectures, M&M, Evidence-Based Medicine, Ethics, and POCUS sessions. Divisional case conferences occur weekly, and additional Quality Improvement and combined M&M conferences are monthly. Multidisciplinary Trauma, ECMO, and Stroke conferences occur quarterly. This is in addition to multiple educational series at the department level. In short, there are a plethora of high-quality learning opportunities for fellows on nearly a daily basis.
Teaching opportunities
Because we believe that effective faculty development must begin during training, we offer our PICU fellows the opportunity to enroll in the Education Scholars Program at OHSU, a highly-regarded longitudinal seminar for motivated and promising clinical teachers.
In addition to this program, there are many opportunities for all PICU fellows to get involved in teaching medical students, residents, nursing staff, and/or other fellows/faculty members. All PICU fellows will alternate teaching informal clinical “chalk talks” to pediatric residents on their PICU rotation on a weekly basis. Other optional teaching opportunities include:
- Pediatric Residency Mock Code (monthly)
- Pediatric Residency Noon Conference (prn)
- PALS instruction (biannual commitment)
- Pediatric Grand Rounds (per invitation)
- PICU nursing education sessions (per invitation)
- PICU division research in progress series (once per fellowship)
- M&M conferences (departmental and divisional, prn)
- Medical student core pediatrics sessions
- Medical student small-group facilitation
Simulation
Our PICU operates the Doernbecher Simulation Program, with a dedicated in-house mannequin named Donnie. Through this program, mock codes are held two-three times monthly, with exposure for both day- and night-shift physicians and staff, in our “native” environment.
The Pediatric Residency Mock Code curriculum also utilizes Donnie, drawing upon the expertise and knowledge of PICU faculty and fellows to guide residents through simulated scenarios.
In addition to their participation in unit-based mock scenarios, and teaching within the pediatric resident mock code curriculum, PICU fellows have regular access to OHSU's state-of-the-art Simulation Center on the South Waterfront, which houses the PALS/ATLS program in addition to Central Line WetLabs and Ventilator Simulations.
Scholarship and mentorship
Training our PICU fellows to become competent physician scientists is a priority of the fellowship program. Fellow scholars meet with the program director and division faculty to delineate research interests within the first several months of fellowship. Significant effort is dedicated to this process to maximize opportunity for a successful investigative career. This is followed by the choice of a research mentor(s) and project, with scholarly activities to commence within the first year of fellowship.
A separate professional mentor is also selected by the fellow early in the first year, to help guide the fellow more generally in the career and personal development.
Additionally, the Pediatric Fellowship Committee, a larger governing body for all pediatric fellowship programs at Doernbecher, provides resources to fellows in project development and choosing a mentor.
OHSU/Doernbecher has a plethora of talented faculty in many areas applicable to pediatric critical care who enjoy mentoring fellows in professional development and scholarly endeavors.
As part of their career development, fellows may choose to pursue an advanced degree, including a Master of Public Health and Master of Clinical Research.
Human Investigations Program (HIP)
All pediatric fellows receive funding to participate in the Human Investigations Program (HIP), a unique and highly-valuable resource for fellowship trainees at OHSU, which is supported by an NIH K30 grant. The HIP is a formal, expertly taught graduate program housed under the Oregon Clinical and Translational Research Institute (OCTRI) and fulfilling all American Board of Pediatrics (ABP) criteria for education in epidemiology, biostatistics, research design, proposal development, and manuscript preparation/review. Fellows also learn to integrate principles of molecular and cell biology, new pharmacology techniques, genomics, and medical informatics into modern clinical, translational, and basic science research. The primary objective of HIP is to increase the competency of physician-scholars in the investigative process, and the coursework is directed toward young investigators and fellows as well as junior faculty. The curricula may result in a Certificate in Human Investigations (one year), or Master of Clinical Research (two years), depending on the career goals of each individual fellow.
Oregon Clinical and Translational Research Institute (OCTRI)
Beyond HIP, OCTRI has a wide array of resources to help investigators and research staff plan and implement successful research studies. OCTRI provides funding and support for novel translational research projects and educational opportunities for faculty, fellows, students, and study coordinators. With major funding from the National Institutes of Health through the Clinical and Translational Science Awards (CTSA), and significant institutional commitment from OHSU and Kaiser Permanente, OCTRI's mission is to improve human health by enhancing clinical and translational research. OCTRI provides a coordinated infrastructure of core research tools. The OCTRI research infrastructure supports investigators with expertise, equipment, facilities, and tools in bioinformatics, biostatistics, community-engaged research, compliance and regulatory support, inpatient and outpatient clinical research, and laboratory analysis. There are many other research centers supporting trainees in research, finding funding, and writing grants.
Recent fellow and alumni peer-reviewed publications
- Exposure to Sedation and Analgesia Medications: Short-term Cognitive Outcomes in Pediatric Critical Care Survivors With Acquired Brain Injury. Drury KM, Hall TA, Orwoll B, Adhikary S, Kirby A, Williams CN.J Intensive Care Med. 2024. PMID: 37885235
- Nonresuscitation Fluid Accumulation and Outcomes After Pediatric Cardiac Surgery: Single-Center Retrospective Cohort Study. Hudkins MR, Miller-Smith L, Evers PD, Muralidaran A, Orwoll BE. Pediatr Crit Care Med. 2023. PMID: 37747301
- Protocol-Driven Initiation and Weaning of High-Flow Nasal Cannula for Patients With Bronchiolitis: A Quality Improvement Initiative. Huang JX, Colwell B, Vadlaputi P, … Siefkes H.Pediatr Crit Care Med. 2023. PMID: 36661418
- Continuing Care For Critically Ill Children Beyond Hospital Discharge: Current State of Follow-up. Williams CN, Hall TA, Francoeur C, Kurz J, Rasmussen L, Hartman ME, O'meara AI, Ferguson NM, Fink EL, Walker T, Drury K, et al; PEDIATRIC NEUROCRITICAL CARE RESEARCH GROUP (PNCRG)..Hosp Pediatr. 2022. PMID: 35314865
- Is Pediatric Intensive Care Trauma-Informed? A Review of Principles and Evidence. Demers LA, Wright NM, Kopstick AJ, Niehaus CE, Hall TA, Williams CN, Riley AR. Children (Basel). 2022. PMID: 36291511
- Prevalence and Risk Factors of Neurologic Manifestations in Hospitalized Children Diagnosed with Acute SARS-CoV-2 or MIS-C. Fink EL, Robertson CL, Wainwright MS, …, Williams CN, Drury K, et al; Global Consortium Study of Neurologic Dysfunction in COVID-19 (GCS-NeuroCOVID) Investigators.Pediatr Neurol. 2022. PMID: 35066369
- Recognizing Pediatric ARDS: Provider Use of the PALICC Recommendations in a Tertiary Pediatric ICU. Kopstick AJ, Rufener CR, Banerji AO, Hudkins MR, Kirby AL, Markwardt S, Orwoll BE. Respir Care. 2022. PMID: 35728822
- Cognitive Dysfunction After Analgesia and Sedation: Out of the Operating Room and Into the Pediatric Intensive Care Unit. Turner AD, Sullivan T, Drury K, Hall TA, Williams CN, Guilliams KP, Murphy S, Iqbal O'Meara AM. Front Behav Neurosci. 2021. 34483858
- A Mixed-Methods Quasi-Experimental Study on Perspectives Among Physicians and Nurses Regarding Use of Palliative Care Teams in the Pediatric Intensive Care Unit After Out-of-Hospital Cardiac Arrest. Broman A, Williams C, Macauley R, Carney PA. Am J Hosp Palliat Care. 2021. PMID: 32638618
- Development and Retrospective Review of a Pediatric Ethics Consultation Service at a Large Academic Center. Leland BD, Wocial LD, Drury K, Rowan CM, Helft PR, Torke AM. HEC Forum. 2020. PMID: 32180057
- Pediatric trauma venous thromboembolism prediction algorithm outperforms current anticoagulation prophylaxis guidelines: a pilot study. Cunningham AJ, Dewey E, Lin S, Haley KM, Burns EC, et al. Pediatr Surg Int. 2020. PMID: 31900592
- PICU Early Mobilization and Impact on Parent Stress. Colwell BRL, Olufs E, Zuckerman K, Kelly SP, Ibsen LM, Williams CN. Hosp Pediatr. 2019. PMID: 30914449
- Mobilization Therapy in the Pediatric Intensive Care Unit: A Multidisciplinary Quality Improvement Initiative. Colwell BRL, Williams CN, Kelly SP, Ibsen LM.Am J Crit Care. 2018. 29716905
- Hospital-to-Home Interventions, Use, and Satisfaction: A Meta-analysis. Hamline MY, Speier RL, Vu PD, Tancredi D, Broman AR, Rasmussen LN, Tullius BP, Shaikh U, Li ST.Pediatrics. 2018. PMID: 3035279
- North American survey on the post-neuroimaging management of children with mild head injuries. Greenberg JK, Jeffe DB, Carpenter CR, Yan Y, Pineda JA, Lumba-Brown A, Keller MS, Berger D, Bollo RJ, Ravindra VM, Naftel RP, Dewan MC, Shah MN, Burns EC, …, Limbrick DD. J Neurosurg Pediatr. 2018. PMID: 30485194
Current fellows

Jordi Morgan, M.D., 2026
Dr. Morgan was born and raised in San Juan, PR until age 15, when he moved to Orlando, FL to finish high school. He attended Brown University in Providence, RI and graduated in 2013 with a concentration in Chemical Biology. After college, Jordi worked as a research assistant and laboratory manager at the Ragon Institute of MGH, MIT & Harvard in Cambridge, MA then moved to NYC where he obtained his MD at the NYU Langone School of Medicine. From there, he completed a residency in Pediatrics at UMass Chan Medical School in Worcester, MA. In his free time, Jordi loves spending time with his dog Tank, traveling, kayaking, riding roller coasters, attending Broadway shows, and playing the latest Legend of Zelda or Pokémon game.

Julia Kononowicz, M.D., 2027

Alyssa Penning, M.D., 2028
Alumni
Brendan Cleary, M.D., 2025
Oregon Health & Science University / Nebraska Children’s
William Clare, M.D., 2025
Rosalind Franklin University of Medicine & Science
V. Divya Nagarajan, M.B.B.S., 2024
Northwestern Medicine/Feinberg School of Medicine
Kurt M. Drury, M.D., M.C.R., 2023
University of Chicago / Comer Children’s Hospital
Matthew Hudkins, M.D., 2022
Oregon Health & Science University / Doernbecher Children’s Hospital
Alia Broman, M.D., 2021
University of New Mexico / UNM Children’s Hospital
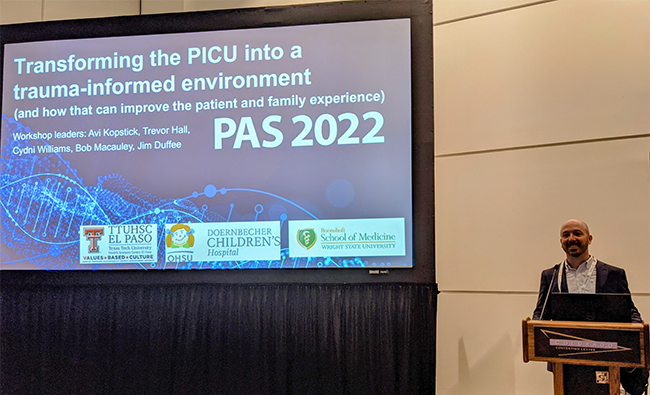
Avi Kopstick, M.D., 2020
University of Texas El Paso / El Paso Children’s Hospital
Theresa Graif, M.D., M.P.H., 2019
University of Oklahoma / Oklahoma Children’s Hospital
Blair Colwell, M.D., 2017
University of California Davis / UC Davis Children’s Hospital
Ashley Jones, M.D., 2016
Mary Bridge Children’s Hospital, Tacoma, WA
Erin Burns, M.D., 2015
Oregon Health & Science University / Doernbecher Children’s Hospital
Faculty
How to apply
Applications to the PCCM Fellowship Training Program must be submitted through the Electronic Residency Application Service (ERAS), and should include the following:
- Personal statement: Please describe how the OHSU PCCM Fellowship Program aligns with you and your career goals; this can be included as a brief addendum to the end of your personal statement.
- At least three letters of recommendation (including one from your residency program director; we do not require a letter from the chair of the department)
- Medical Student Performance Evaluation (MSPE)
- Medical school transcript
- USMLE and COMLEX scores
International graduates:
Applicants to OHSU’s PCCM Fellowship program must have completed a US Residency program by the time of matriculation. Applicants must be legally able to work in the US, or eligible to obtain work. Applicants must also provide a copy of a valid certificate from the Educational Commission for Foreign Medical Graduates, participate in the National Resident Matching Program (NRMP) and apply through ERAS.
Please also see the OHSU GME information on Applying to OHSU Residencies and Fellowships.
Oregon Health and Science University values a diverse and culturally competent workforce. We are proud of our commitment to being an equal opportunity, affirmative action organization that does not discriminate against applicants on the basis of any protected class status, including disability status and protected veteran status. Individuals with diverse backgrounds and those who promote diversity and a culture of inclusion are encouraged to apply. To request reasonable accommodation contact the Office of Civil Rights Investigations and Compliance at 503-494-5148 or ocic@ohsu.edu.
Application Deadline: We apologize that we cannot review applications received after early August.
Interviews
Applicants are invited for an interview based on holistic review of their application. All interviews will be conducted virtually until further notice. Timing of interviews will range from September to November.
Upon receipt of an application, our selection committee will review and notify each applicant by email of the decision to interview. Decisions may take several weeks. Applicants may then schedule an interview online through Thalamus. Unfortunately, due to the volume of applications, we are unable to interview all applicants.
Invited applicants will virtually meet 1-on-1 with up to 4 faculty members during a half-day session of interviews (morning or afternoon.) Program Overview and Virtual Tour videos will be made available to invitees to review asynchronously. Additionally, these candidates will be invited to attend one of several informal Q&A sessions with the PD and current fellows.
After your interview
We hope that you find your virtual interview experience with us to be informative, efficient and enjoyable! Please do not hesitate to contact us with any follow-up questions.
Fellowship Coordinator: Sarah Nolte, M.S., C-TAGME nolte@ohsu.edu
Program Director: Erin Burns, M.D. comer@ohsu.edu
We are happy to provide additional emails for faculty and fellows upon request.
Written correspondence to anyone you met can be mailed to:
Oregon Health & Science University
Mail Code CDRC-P
707 S.W. Gaines Street
Portland, OR 97239
Our commitment to diversity, equity, and inclusion
We welcome everyone.
- All races
- All religions
- All countries of origin
- All sexual orientations
- All genders
- All abilities
This is in the larger context of a University that strives for the same. OHSU’s Diversity, Equity, Inclusion and Belonging Diversity, Equity, Inclusion and Belonging (DEIB) leads and supports university-wide initiatives to create an environment of respect and inclusion for all people. This includes Stepping in for Respect for all campus faculty, staff and trainees, with a goal of mitigating the effects of unconscious bias in our everyday interactions and behaviors.
Being a patient or provider in a pediatric intensive care unit is stressful enough. It is absolutely our duty to strive to mitigate any added stress from inequities or microaggressions in our fellowship and unit.
Contact us
Erin C. Burns, M.D.
Fellowship Program Director
comer@ohsu.edu
Sarah Nolte, M.S., C-TAGME
Program Technician
nolte@ohsu.edu
