Pediatric Aerodigestive Care

Aerodigestive disorders occur when children get food into their lungs or airways, causing chronic (ongoing) breathing problems. At OHSU Doernbecher Children’s Hospital, we provide coordinated care to give your child the best possible treatment.
We offer:
- A team approach to care, with doctors from multiple specialties working together to treat your child
- A full range of child specialists
- The only pediatric aerodigestive center in Oregon and southwest Washington
Understanding aerodigestive conditions
What are aerodigestive conditions?
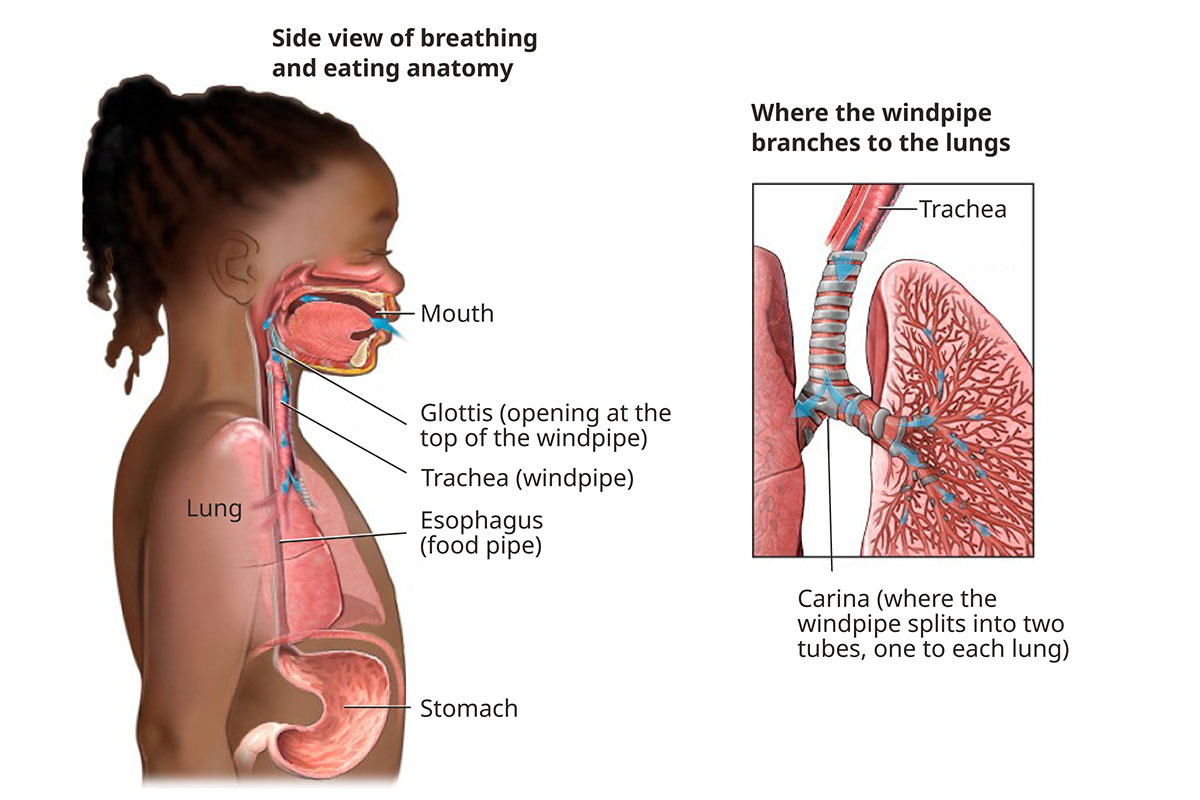
An aerodigestive disorder is a combination of conditions that affects your child’s breathing, swallowing or growth. It occurs when the pathways used for breathing and swallowing let food or liquid into the lungs. Children with such a disorder typically have frequent respiratory illnesses.
Examples:
- A child has asthma that doesn’t respond to medication. The doctor learns that the child always coughs after drinking fluids. If some of the fluid is getting into the lungs or blocking an airway, the child may have an aerodigestive disorder.
- A child with a complex genetic syndrome or neurologic disorder such as multiple sclerosis can develop an aerodigestive disorder. As a child with MS gets older, for example, weakened muscles make it harder to swallow food. This can lead to an aerodigestive disorder.
Pediatric Respiratory and Digestive Anatomy and Function
Health issues
Aerodigestive disorders are complicated. Patients often have multiple health issues such as:
Dysphagia: This condition makes swallowing difficult or painful. It feels like food or liquid is stuck in the throat. When eating is hard, a child can become unable to eat enough to stay healthy. Dysphagia may occur in children born with swallowing abnormalities.
Asthma: This lung inflammation makes it difficult to breathe.
Eosinophilic esophagitis: This is inflammation or irritation of the esophagus (food pipe). It can cause pain, nausea, spitting up (regurgitation), vomiting and trouble swallowing.
Obstructive sleep apnea: In this condition, the soft tissue in your child’s throat blocks the upper airway during sleep. This cuts off oxygen for a few seconds until the child wakes up and breathes normally.
Aspiration: When food or liquid enters the airways. Types are:
- Swallowing aspiration, when food goes into the airway and lungs instead of the stomach.
- Reflux aspiration, when stomach acid backs up into the airway and lungs.
Chronic cough: A cough that lasts for four weeks or longer.
Bronchomalacia: Bronchial tubes that let air into your child’s lungs collapse and can’t stay open when exhaling. Doctors sometime refer to this as a “floppy” windpipe. It causes secretions to get trapped and infected.
Upper airway obstruction: This is a blockage in the trachea (windpipe), voice box and throat that prevents your child from getting enough oxygen.
Pneumonia is a lung infection. It's called recurrent pneumonia when it happens at least twice a year.
Tracheoesophageal fistula: A birth defect results in an abnormal connection between the esophagus (food pipe) and windpipe, sometimes causing breathing problems.
Tracheomalacia: The windpipe is softer than normal, sometimes because of a birth defect. It can cause the child’s airway to collapse, leading to breathing problems.
Bronchopulmonary dysplasia: This chronic lung disease affects mainly premature babies who required mechanical ventilation and oxygen. Lung damage is caused by long-term use of oxygen and a respirator.
Diagnosing aerodigestive conditions
Your child’s doctor will get your child’s medical history and do a physical exam. Additional tests may include:
Chest X-ray: A baseline X-ray is done to assess the condition of your child’s lungs.
Modified barium swallow study: Radiology and speech specialists use a type of X-ray to track colored liquid as it travels through your child’s body. This shows whether the liquid goes into the stomach or gets into the airway.
Pulmonary function testing: A series of breathing tests measure how well your child’s lungs are working. Your child blows into a mouthpiece that measures how air moves in and out of the lungs, and how big and strong the lungs are.
Fiberoptic endoscopic evaluation of swallowing (FEES): In this procedure, a small flexible tube with a camera at the tip is placed through your child’s nose to watch how the mouth and throat respond to swallowing. The test lets doctors see if liquid is going into the airway or getting stuck.
CT scan: Computed tomography imaging, also called a CT scan, captures highly detailed images inside the lungs and airways to check for damage.
Sweat chloride test for cystic fibrosis: The painless test measures the amount of salt (sodium chloride) in sweat. Newborns and children with cystic fibrosis have a higher level. Your child’s doctor may request this test if the doctor suspects cystic fibrosis.
Sleep test: A polysomnogram (PSG) is an overnight test in our sleep lab to measure and record how your child is sleeping. If your child’s doctor thinks a sleep disorder may be causing your child’s aerodigestive issues, a sleep test will be done to check for sleep apnea or another sleep disorder.
Complete care
- Specialists meet before and after each visit with your child to create a personal treatment plan.
- A nurse practitioner meets with families to present the care plan.
- A team of schedulers guides families through procedures and clinic visits.
- Multiple procedures are done during one hospital visit under a single sedation.
- Your child’s care team may include a range of child specialists, if needed, including:
- A pulmonologist
- An otolaryngologist (ear, nose and throat surgeon)
- A gastroenterologist (digestive system doctor)
- A speech-language pathologist
- A pediatric surgeon
- A dietitian
Treatments for aerodigestive conditions
Our doctors treat a wide variety of aerodigestive conditions. The three main ones include:
Dysphagia
Liquid thickeners: A starch product is added to liquids to make them thicker. This helps liquids move into the stomach instead of the lungs. A child with a swallowing problem typically also finds thicker liquids easier to drink. In some children, this resolves the issue over time.
Surgery: Surgery can repair a gap between the voice box and food pipe (laryngeal cleft), stopping food from going into the lungs.
Tube feeding: A temporary nasogastric tube is placed through your child’s nose and down into the stomach, making sure food goes directly to the stomach. Families are taught how to replace the tube.
Reflux
Medication:
- Acid suppression: Antacids, histamine 2 blockers and proton pump inhibitors taken as tablets or pills reduce and prevent acid in your child’s stomach.
- Promotility drugs: These medications help food move out of the stomach or gut faster.
Food thickeners: Thickeners can make food easier to swallow.
Tube feeding: A temporary nasojejunal tube is placed through your child’s nose, down the throat, past the stomach and into the upper intestines (jejunum). Keeping food out of the stomach reduces the amount of fluid that can reflux.
Surgery: Minimally invasive surgery (Nissen fundoplication) involves wrapping part of the stomach around the lower food pipe opening to prevent acid reflux.
Obstructive sleep apnea
Surgery: Surgery to remove enlarged tonsils and adenoids is a common treatment for children with obstructive sleep apnea. If a child has unusual facial anatomy, we may consider other options, such as craniofacial surgery.
CPAP (continuous positive airway pressure): A CPAP machine improves breathing at night. The child wears a mask over the nose that’s connected by a hose to a machine that gently blows air. Your child’s doctor determines the air pressure to keep the airway open.
BPAP (bilevel positive airway pressure): This machine, similar to a CPAP, helps some children exhale. It uses higher air pressure for inhaling and lower pressure for exhaling.
Medication: Nasal steroids and other medications may be prescribed to help open airways and ease your child’s breathing.
Learn more
- Pediatric Dysphagia, American Speech-Language-Hearing Association
- Pediatric Sleep-disordered Breathing, American Academy of Otolaryngology
Location
OHSU Doernbecher Children’s Hospital, seventh floor
700 S.W. Campus Drive
Portland, OR 97239
Free parking for patients and visitors
Refer a patient
- Refer your patient to OHSU Doernbecher.
- Call 503-346-0644 to seek provider-to-provider advice.