A collaboration among OHSU cancer researchers reveals which cases of ocular melanoma are likely to spread.
Ocular melanoma is a relatively rare cancer, with just 5 or 6 cases per million people per year in the United States. But in adults, it is the most common primary eye tumor, and it is aggressive. By the time many patients are evaluated, micrometastasis has already occurred. This means that despite successful treatment of the tumor in the eye, patients die from distant spread of their disease.
Though ocular melanoma typically arises in older adults, ocular oncologist Alison Skalet, M.D., Ph.D., emphasizes that it can happen at any age. “We treated an 18-year-old with ocular melanoma on my first day of clinical fellowship at Casey Eye Institute,” she says.
Unfortunately, only a few years later, the patient died. Now, Skalet and colleagues at the OHSU Knight Cancer Institute have published research that could have allowed them to noninvasively predict whether the patient’s tumor would metastasize, enabling them to make important choices about treatment and quality of life.[1]
A handful of challenges
While ocular melanoma is treatable, there is currently no way to detect micrometastases. Current surveillance is via imaging of the lungs and liver with MRI, CT or ultrasound. “This can go on for years,” Skalet says. “The uncertainty is difficult to live with.” Patients must adjust to the knowledge that they could face advanced cancer at any time.
Hybrid cells provide a clue
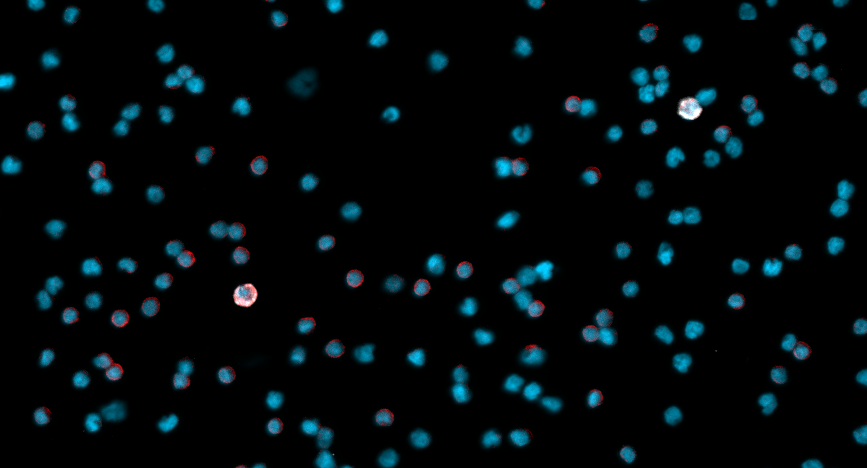
Skalet is involved with the OHSU Knight Cancer Institute’s melanoma program, and it was through a collaboration with colleague Melissa Wong, PhD, that she discovered circulating hybrid cells, or CHCs, present in the blood of patients treated for ocular melanoma. These cells provide important clues about disease stage and metastasis.
“Graduate student Charlie Gast found that cancer cells and immune cells spontaneously fused in vitro,” Skalet explains. “These cells were hybrids, sharing both phenotypic and genotypic identities with the two types of cells. The Wong lab has shown that the result is CHCs -- cancer cells with enhanced migratory function and tumorigenicity.” This original research was published in 2018,[2] and so far, CHCs have been found in patients with more than 14 types of cancer.
Skalet and Wong looked for hybrid cells in the blood of patients with ocular melanoma. They found CHCs in much greater numbers than the circulating tumor cells, or CTCs, traditionally used as a marker.
An aid to prognosis
CHC levels have promise as a prognostic biomarker. “Currently, we have excellent molecular prognostic testing based on tumor tissue,” Skalet explains. However, some tumors are difficult to biopsy and patients may choose to avoid biopsy due to surgical risk. Biopsy of tumor tissue alone may miss variability that is clinically important. In addition, once the primary tumor is treated, repeat biopsy is not possible.
In the 2022 study, measuring levels of CHCs at the time of diagnosis was shown to predict which patients develop metastatic disease. “In the future, we could have a non-invasive way of identifying which patients will have disease progression and doing risk stratification for clinical trials. We would also have the option to re-test CHC levels over time to assess treatment responses,” Skalet says.
Potential as a diagnostic tool
“We are also interested in evaluating CHCs as a diagnostic biomarker,” says Skalet. “Can they help us diagnose ocular melanoma, or differentiate melanoma from benign nevi based on a blood test?” If so, CHC levels could be measured in patients who have indeterminate tumors that cannot readily be categorized as benign or aggressive. While this work is in early stages, “CHCs have potential to improve diagnostic certainty in the future,” Skalet says.
Measuring treatment effectiveness, predicting therapeutic vulnerabilities
Circulating hybrid cells may also be a marker of how well treatment is working. “ Do CHC levels drop after treatment?” Skalet asks. “This is an exciting area of ongoing research.”
Casey Eye Institute treats many patients with ocular melanoma – approximately 4 percent of those in the United States, according to Skalet. At OHSU she works with a multi-disciplinary team to provide care to patients with ocular melanoma.
A new treatment option for patients with metastatic ocular melanoma suggests how this could work. In January 2022, the US Food and Drug Administration approved the first-ever drug for ocular melanoma, tebentafusp-tnb (KIMMTRAK). This treatment is available through medical oncology at OHSU to patients who qualify.
“This is the first drug to ever improve survival,” Skalet says. However, there is a caveat. “Only about 50 percent of patients are candidates for it, because you need a specific HLA blood type to benefit from this immunotherapy. More treatments options are needed.” Skalet is fascinated by the potential for CHCs to provide clues that may lead to new treatments in the future. “[CHCs] are a novel cell type that we believe is driving metastasis,” she says. “Evaluating CHC susceptibilities may lead us to new treatment approaches.”
Next steps
Skalet recently received funding from the Knight Cancer Institute to further explore CHCs in uveal melanoma patients, focusing on how CHCs may provide clues regarding treatment options. She and Wong will be soon be applying for NIH funding as well. She says, “We have many exciting research opportunities building upon our early work. I am eager to see how we can ultimately expand knowledge in this new area and how we can translate our discoveries into improved patient care.”
As a major center for the care of uveal melanoma, Casey Eye Institute’s team, led by Skalet, aims to bring the latest ocular melanoma research and clinical trial opportunities to OHSU. This will give patients in the region the most comprehensive treatment options and help develop knowledge that benefits patients and clinicians far beyond Casey Eye Institute.
[1] Parappilly MS, Chin Y, Whalen RM, et al. Circulating neoplastic-immune hybrid cells predict metastatic progression in uveal melanoma. Cancers (Basel). 2022;14(19):4617. Published 2022 Sep 23. doi:10.3390/cancers14194617
[2] Gast CE, Silk AD, Zarour L, et al. Cell fusion potentiates tumor heterogeneity and reveals circulating hybrid cells that correlate with stage and survival. Sci Adv. 2018;4(9):eaat7828. Published 2018 Sep 12. doi:10.1126/sciadv.aat7828