Understanding Deep Brain Stimulation (DBS)

Deep brain stimulation, or DBS, has helped thousands of patients with Parkinson’s disease or essential tremor.
Important things to know:
- DBS works by regulating abnormal signals in the brain.
- It is safe and effective.
- It is not a cure, and not everyone is a good candidate for DBS.
Deep Brain Stimulation
How does DBS work?
DBS is a surgical procedure that can help some people with movement disorders. The Food and Drug Administration has approved DBS to treat Parkinson's disease and essential tremor.
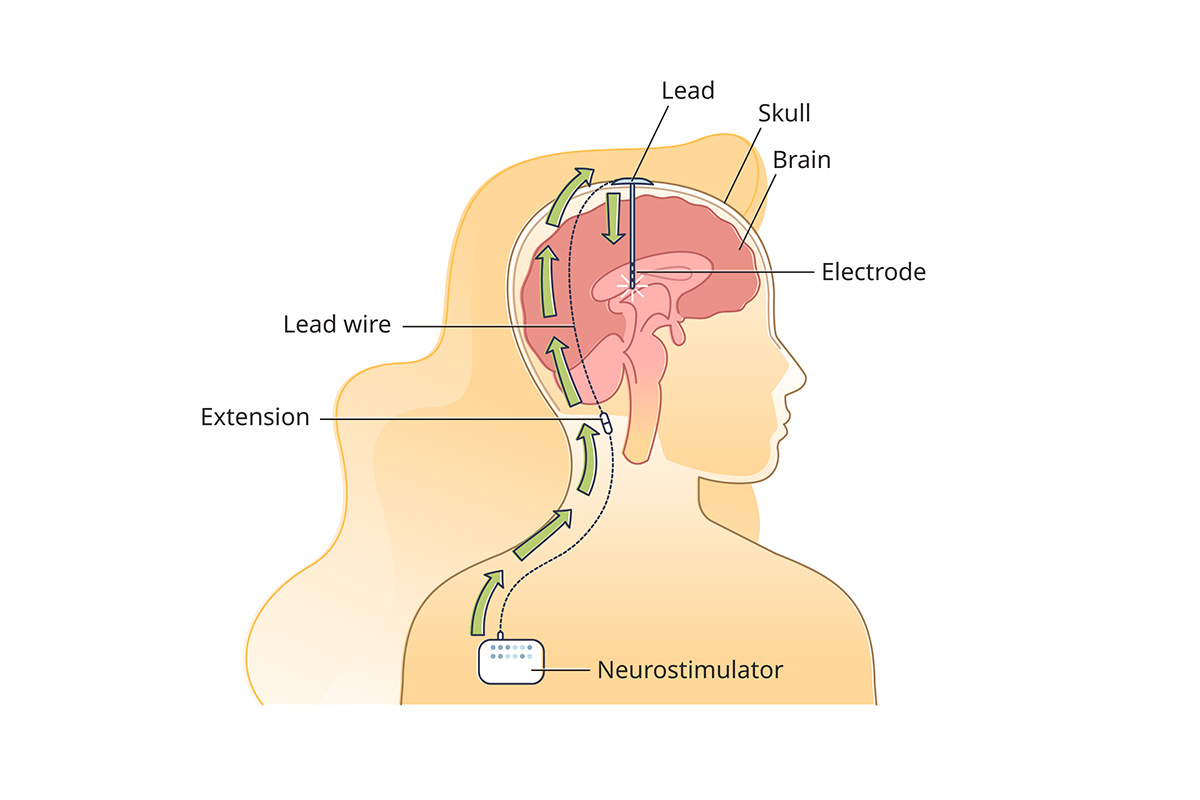
DBS is a minimally invasive procedure. First, surgeons place small electrodes in certain areas of your brain. About a week later, surgeons place an IPG (implanted pulse generator) device under the skin of your chest, below your collarbone. Wires under your skin connect the IPG to the electrodes in your brain. The IPG sends electrical pulses to the electrodes, regulating signals in that area of the brain.
Experts believe that the low-voltage pulses of electricity from DBS regulate abnormal nerve signals in your brain. The pulses also might change brain chemicals that cause the tremors and other symptoms. Experts are still researching exactly how DBS works.
OHSU’s Dr. Kim Burchiel, who leads our team, was the first surgeon in the United States to perform DBS for Parkinson’s disease, in 1991. He pioneered “awake” DBS in 2011, giving patients a more precise and more comfortable option.
What’s the difference between asleep DBS and awake DBS?
For many years, DBS patients were awake during the procedure. Awake DBS is still done at many hospitals. Patients have numbing medication and feel no pain. But they must be awake for at least part of the procedure so they can give responses that help the neurosurgeon put the electrodes in exactly the right places in the brain.
Dr. Burchiel innovated asleep DBS in 2011, with the patient under general anesthesia. He and his team use high-resolution brain scans taken before and during surgery to precisely place the electrodes in the brain. Asleep DBS is faster, safer and more accurate. OHSU now performs only asleep DBS.
Is DBS safe?
DBS is surgery, and all surgery has risks. But DBS risks are low. A three-year study of DBS procedures found that among 2,038 patients who had DBS, seventy-two had complications, and one died. Among the 219 patients in the study who had DBS at OHSU, none died and one had complications.
How long has DBS been used?
Dr. Burchiel's first DBS procedure for Parkinson’s in the U.S., in 1991, was part of a clinical trial (a test on people who give consent). At the time, DBS was not available to the public. The FDA approved DBS as a treatment for essential tremor in 1997. It approved DBS for Parkinson’s disease in 2002.
Who is a good candidate for DBS?
DBS is not right for everyone with essential tremor or Parkinson's disease. It is most helpful if at least one of these situations applies to you:
- Your medication is not controlling your symptoms, or it’s not working as well as it used to.
- You need to take medication more often, or in higher doses, to get some control of your symptoms.
- Your medication is causing severe side effects, keeping you from taking enough to control your symptoms.
- For Parkinson's disease patients, you have idiopathic or classic Parkinson's. DBS does not help other types of Parkinson's.
What are the benefits of DBS?
DBS can:
- Improve your quality of life by reducing tremor and improving your motor function.
- Work 24 hours a day, so you depend less on medication to control your symptoms. You may still take medication if it helps.
- Be adjusted. Your DBS team can change the settings on your implanted pulse generator to make it more effective and to reduce any side effects.
- Be reversed. Your DBS team can turn off the implanted pulse generator so you can try new treatments that become available.
- Continue working for years. The batteries in the implanted pulse generator last three to five years. We replace them in a minor outpatient procedure. Newer rechargeable generators last about 15 years before they need replacement.
What are the risks of DBS?
DBS is a safe procedure that rarely has complications. But any surgery has risks. With DBS, risks include:
- Infection
- Bleeding in the brain
- Stroke
- Part of the DBS system breaking
- The implanted pulse generator not working
What happens during and after DBS surgery?
Deep brain stimulation surgery involves two procedures, two days to one week apart. We often call them Stage 1 and Stage 2.
Stage 1: This procedure takes about three hours.
We give you general anesthesia so you are asleep. We make one or two incisions in your skull, each smaller than a dime.
We use advanced scans of your brain taken before and during surgery to help us place small electrodes in precise parts of your brain that control movement. Some DBS systems have two electrodes; some have one electrode.
We tuck thin wires from the electrodes under the skin above and behind your ear. The wires are attached to the implanted pulse generator in Stage 2.
Most patients spend one night in the hospital.
Stage 2: This procedure takes about 45 minutes for each electrode.
We give you general anesthesia and place the implanted pulse generator (IPG) under the skin of your chest, just below your collarbone. The generator is about the size of a tea bag. We attach the wires placed in Stage 1 to the generator. Right after surgery, we test your IPG and then turn it off. Our DBS team will turn on and program your IPG after you recover.
Most patients go home the same day.
After surgery: About one month after Stage 2, you return to our clinic to program your IPG. We will adjust the electrical impulses so they work best to treat your symptoms. Your local neurologist may be able to do some or all of your IPG programming. Many patients need several sessions, usually a month apart, to find the best symptom control. Learn more about what to expect after DBS surgery
Preparing for surgery
Your DBS team will give you and your family detailed instructions before surgery. This includes things to do and things to avoid so surgery is as safe as possible.
It’s important to let your care team know about all of your medications and medical conditions. Do not stop taking any of your medications without speaking with your primary care or other provider. You will need to stop taking certain medications before surgery, including:
- Warfarin (brand name Coumadin)
- Plavix
- Ibuprofen
- Naproxen (brand names include Naprosyn and Aleve)
- Aspirin, and any medications that contain aspirin
You can take Tylenol and other medications with acetaminophen in the days and weeks before surgery.
For patients
- Ask questions
- Arrange a referral from your neurologist
- Schedule follow-up appointments
Download our patient guides:
Location
Parking is free for patients and their visitors.
Center for Health & Healing
Building 1, eighth floor
3303 S. Bond Ave.
Portland, OR 97239
Map and directions
Refer a patient
- See our Referring Providers page to learn about making a referral to OHSU, how we partner with you, and training opportunities.
- Is your patient a candidate for DBS?
- Download our DBS guide for providers.
- Call 503-494-4567 to seek provider-to-provider advice.