Understanding Pediatric Brain and Spinal Cord Tumors
Brain and spinal cord tumors in children
Learning more about brain and spinal cord tumors in children and teens can help make a scary diagnosis less so. These tumors vary tremendously by individual, however. If your child has a brain or spinal cord tumor, please talk with your Doernbecher care providers about questions or concerns. They are in the best position to assess your child’s unique condition.
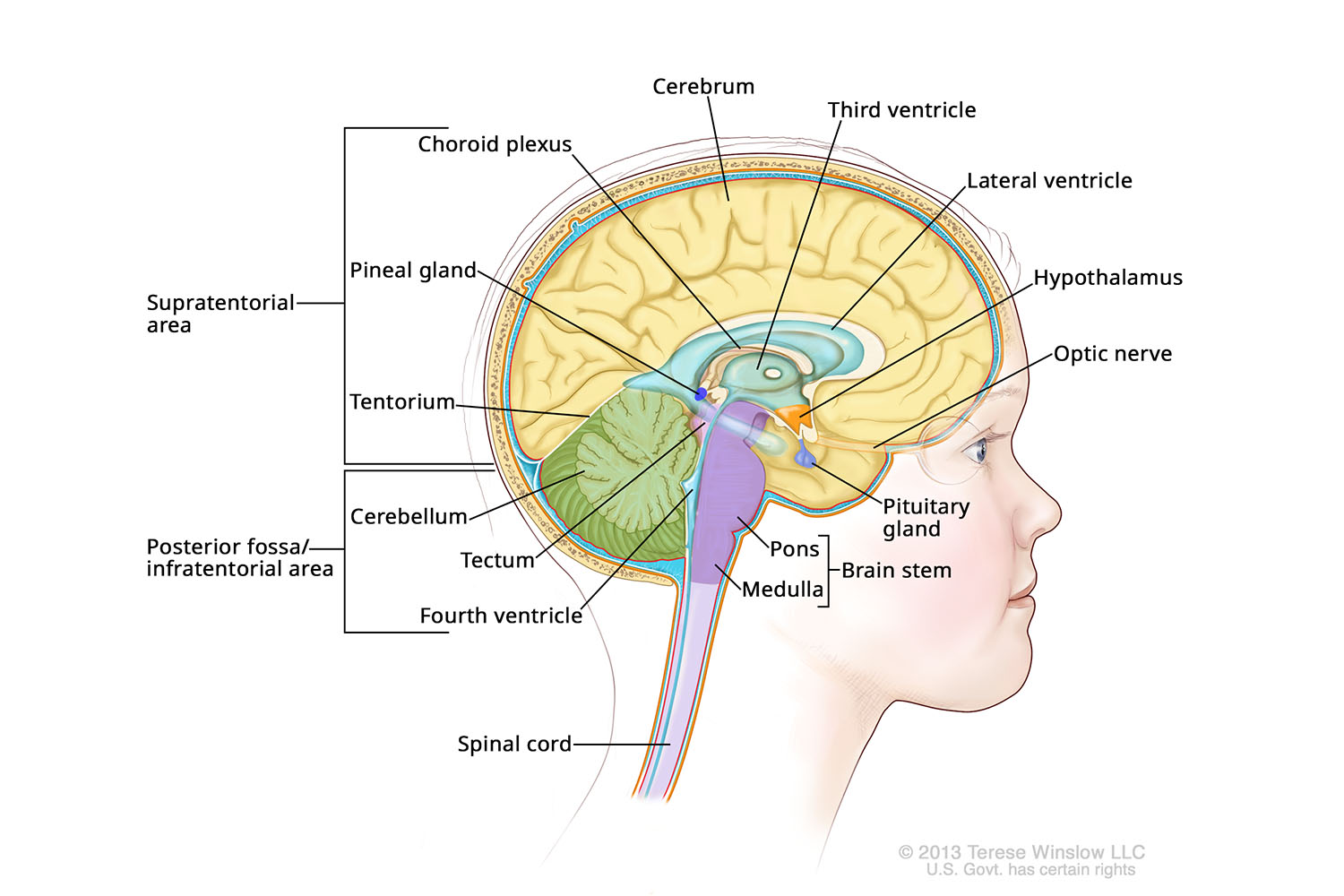
Anatomy of the Brain (Medial)
Brain and spinal cord tumors in children
What are tumors?
Tumors are masses of abnormal cells. Only some tumors are cancer. Brain and spinal cord tumors are “solid” tumors, unlike blood cancers such as leukemia. They also behave much differently in children than in adults, making pediatric specialists especially important. The cause of most brain tumors is unknown, as is any way to prevent them.
How common are they?
Brain and spinal cord tumors are rare, occurring in fewer than six in 100,000 U.S. children and teens. At the same time, they are the most common solid tumor in children, and the second most common cancer in children after leukemia.
More than 4,500 U.S. children are diagnosed with a brain or spinal cord tumor each year. The majority are cured, though rates vary widely depending on the tumor type and many other factors.¹
How are they categorized?
Because the brain and spinal cord make up the central nervous system, these tumors are also called CNS tumors. CNS tumors are very complex. The World Health Organization recognizes more than 150 types.
The field is also evolving as researchers at OHSU and beyond identify ways to fight tumors at the molecular level.² Here are some other ways these tumors are categorized:
Benign or malignant
Benign: Not cancer. These tumors grow slowly, are generally not invasive and typically have clear edges that make them easier to remove. They still pose serious health threats in the brain and spinal cord, though, because they can press on vital structures.
Malignant: Cancer. These tumors contain abnormal, rapidly dividing cells that can invade normal tissue. Brain and spinal cord tumors rarely spread outside the central nervous system, but they are particularly concerning because they can damage essential functions.
Where it developed
Primary tumor: A tumor discovered where it developed. (With brain and spinal cord tumors in children, the primary tumor can also mean the main or largest tumor.)
Secondary tumor: A tumor that spread from elsewhere in the body. These are also called metastatic brain tumors because they “metastasized” from elsewhere. They are treated differently than primary tumors. (With brain and spinal cord tumors in children, a secondary tumor can also mean a smaller tumor in the central nervous system.)
New, recurrence or progression
New: This is a tumor that's newly discovered and unrelated to any previous tumor.
Recurrence: After a tumor is treated, it may shrink or vanish. If it returns, it’s called a recurrence. Tumors can recur one or more times, in the same place or somewhere else. Some recurring tumors are managed as a chronic illness over years.
Progression: This describes when a tumor grows. Often, it's used to describe growth of a "residual" tumor, or the tumor left after treatment. A residual tumor, for example, can be the part of a tumor that could not be surgically removed.
Cell type
Brain tumors are often classified by the type of cells they originated in. Some arise from “glial” cells, for example, or the brain cells that support neurons. See the section on brain tumor types to learn more.
Grade
Brain tumors are graded on a scale of one to four. The lower the grade, the less aggressive the tumor and the easier it is to treat.
Tumors graded I or II are typically “low grade” and benign (not cancer). Tumors graded III and IV are “high grade” and malignant (cancer). Low-grade tumors sometimes, though rarely, develop into high-grade tumors. A type of doctor called a pathologist determines the grade by looking at samples of the tumor under a microscope.
Here’s how the World Health Organization defines grades³.
- Grade I: Slow-growing. Cells look almost normal. Associated with long-term survival. Rare in adults.
- Grade II: Relatively slow-growing. Cells look slightly abnormal. Can spread to nearby normal brain tissue and recur, sometimes as a higher-grade tumor.
- Grade III: Cells look abnormal and are actively reproducing. They can grow into nearby normal brain tissue and are prone to recurring, often as a grade IV tumor.
- Grade IV: Cells look highly abnormal and rapidly reproduce. Tumors form new blood vessels to support growth. They have dead cells (necrosis) in their centers. They can easily invade nearby normal brain tissue.
Stage
A tumor's stage is another way to measure how serious it is based on factors such as size, location, grade and whether it has spread. The lower the stage, the less serious.
Staging is not commonly used for brain and spinal cord tumors, however, because these tumors are so different from other types of tumors. For brain and spinal cord tumors, spread is the most important factor.
Still, because many patients and families have questions about a tumor's stage, we're providing a common staging system from the National Cancer Institute⁴:
- Stage 0: Abnormal cells are present but haven’t spread.
- Stages I, II and III: Cancer is present. A higher stage indicates that the tumor is bigger and has invaded more nearby tissue.
- Stage IV: The cancer has spread to other parts of the body. (Brain and spinal cord tumors rarely spread outside the central nervous system. They can spread within the system through cerebrospinal fluid, the liquid that cushions the brain and spinal cord from injury.)
Brain tumor types
Here is a simplified system for understanding the most common types of childhood brain tumors. This classification is based on the type of cells the tumor originated in. Tumors can also be “mixed-cell,” arising from more than one type of cell. Some of the following types also have several subtypes.
Gliomas
Gliomas are tumors that originate in glial cells, one of the two main types of cells in the central nervous system. These cells are also called “non-neuronal” because they aren’t neurons, the other main type. Glial cells surround and support neurons. Types include oligodendrocytes, astrocytes and ependymal cells.
Gliomas make up about half of childhood brain tumors, according to the American Cancer Society. Many are low grade and highly curable, while others are high grade and require aggressive treatment.
Types include:
Astrocytoma: This tumor originates in the star-shaped astrocyte cells, often in the cerebellum, which controls movement, posture and balance. Some forms, such as pilocytic astrocytoma, are low grade and rarely invade other tissue. Others, such as glioblastoma, are fast-growing and invasive.
Oligodendroglioma: This low-grade tumor originates in oligodendrocytes, most commonly in the cerebrum, the upper part of the brain that controls higher functions such as reasoning and memory. Oligodendrogliomas account for about 1 percent of childhood brain tumors, according to the American Cancer Society.
Ependymoma: This type of tumor develops in the ependymal cells, which line the brain’s fluid-filled ventricles (cavities) and the center of the spinal cord. They range from low to high grade. They rarely invade other brain tissue, making some curable with surgery. Types that spread through cerebrospinal fluid are more difficult to treat. Ependymomas account for about 5 percent of pediatric brain tumors, according to the American Cancer Society.
Neuronal tumors
These tumors arise from neurons, or nerve cells. Neurons are at the root of all thought, movement and sensation. They use electrochemical signals to transmit messages between parts of the brain, and between the brain and the rest of the nervous system.
Medulloblastoma: This is the most common malignant brain tumor in children, accounting for about one-fifth of cases, according to the American Brain Tumor Association. These aggressive tumors occur in the cerebellum, at the base of the brain. They are divided into four subgroups, each with distinct features requiring different treatment. Research is shedding light on their molecular pathways, opening new ways to fight them.
Pineoblastoma: This malignant tumor arises in the pea-size pineal gland at the center of the brain. The pineal gland produces melatonin, a hormone that helps regulates the sleep-wake cycle and some reproductive hormones. Pineoblastomas are more aggressive than other tumors that develop in this gland.
Supratentorial primitive neuroectodermal tumor: This tumor occurs in the upper part of the brain called the cerebrum. Supratentorial means the tumor is above the tentorium, a sheet of tissue that divides regions of the brain.
Atypical teratoid/rhabdoid tumor, or AT/RT: This fast-growing, malignant tumor is relatively rare and usually found in children age 3 or younger. It commonly occurs in the posterior fossa, a cavity in the lower back of the skull that encases the brain's cerebellum and brain stem.
Choroid plexus tumors
The choroid plexus lines the brain’s fluid-filled ventricles and produces cerebrospinal fluid, or CSF. These tumors are relatively rare overall but make up 10 to 20 percent of brain tumors found in children up to age 1, according to the American Brain Tumor Association.
Choroid plexus papilloma: This benign tumor is the most common type. It is slow-growing and rarely spreads. It can block CSF or cause the brain to produce too much CSF, causing the pressure and fluid buildup known as hydrocephalus.
Choroid plexus carcinoma: The malignant form can be aggressive, with a tendency to grow and to spread via CSF pathways.
Germ cell tumors
These tumors arise from germ cells, or reproductive cells that are supposed to migrate to the testicles to become sperm or to the ovaries to become eggs. Some travel to the brain in error and develop into tumors.
Germ cell tumors account for 3 to 5 percent of pediatric brain tumors, according to the American Brain Tumor Association. They are often found in the pineal gland, most commonly in teens. Less often, they develop in the area of the pituitary gland, which controls growth and other vital hormones. Most germ cell tumors are malignant but curable.
Germinoma: This is the most common germ cell tumor in the brain. It looks like testicular or ovarian cancer under a microscope but is typically highly treatable.
NGGCT, or a nongerminomatous germ cell tumor: This type includes several subtypes. They are made up of a greater variety of cells than germinomas. They are also more likely to spread into cerebrospinal fluid and are generally more difficult to treat.
Craniopharyngioma
This benign, slow-growing tumor develops in the area of the pituitary gland, which controls growth and other important hormones, and the optic nerves, which transmit information from the eyes to the brain.
They often contain a mix of fluid and tissue, and they can grow large before they are diagnosed. They account for 5 to 10 percent of childhood brain tumors, according to the American Brain Tumor Association.
Craniopharyngiomas can cause problems by pressing on the pituitary gland, disrupting hormones and sometimes stunting growth; by blocking CSF, causing hydrocephalus; or by pressing on optic nerves, damaging vision.
Learn more
¹ Central Brain Tumor Registry of the United States
² Acta Neuropathologica
³ American Brain Tumor Association
⁴ National Cancer Institute
Location
Parking is free for patients and their visitors.
Doernbecher Children’s Hospital
700 S.W. Campus Drive
Portland, OR 97239
Map and directions
Refer a patient
- Refer your patient to OHSU Doernbecher.
- Call 503-346-0644 to seek provider-to-provider advice.