Pelvic Organ Prolapse
Pelvic prolapse, the loss of support to your pelvic organs, is common as we age. The OHSU Center for Women’s Health offers leading-edge care that will help you get back to your regular activities.
You’ll find:
- A team of top experts working together to create the best care plan for you
- A complete evaluation of all your pelvic organs using the latest tests and technology
- Effective treatment options, such as physical therapy, that don’t involve surgery
- Minimally invasive surgeries for quicker recovery
Understanding pelvic organ prolapse
What is pelvic prolapse?
Pelvic prolapse is the loss of muscle and tissue support to your vagina, uterus, bladder or rectum. Without support, one or more of these organs can drop from their regular position. This can cause discomfort, urine leaks or bowel problems.
Prolapse becomes more common with age. It can range from a slight drop to a bulge you can see or feel outside your vagina.
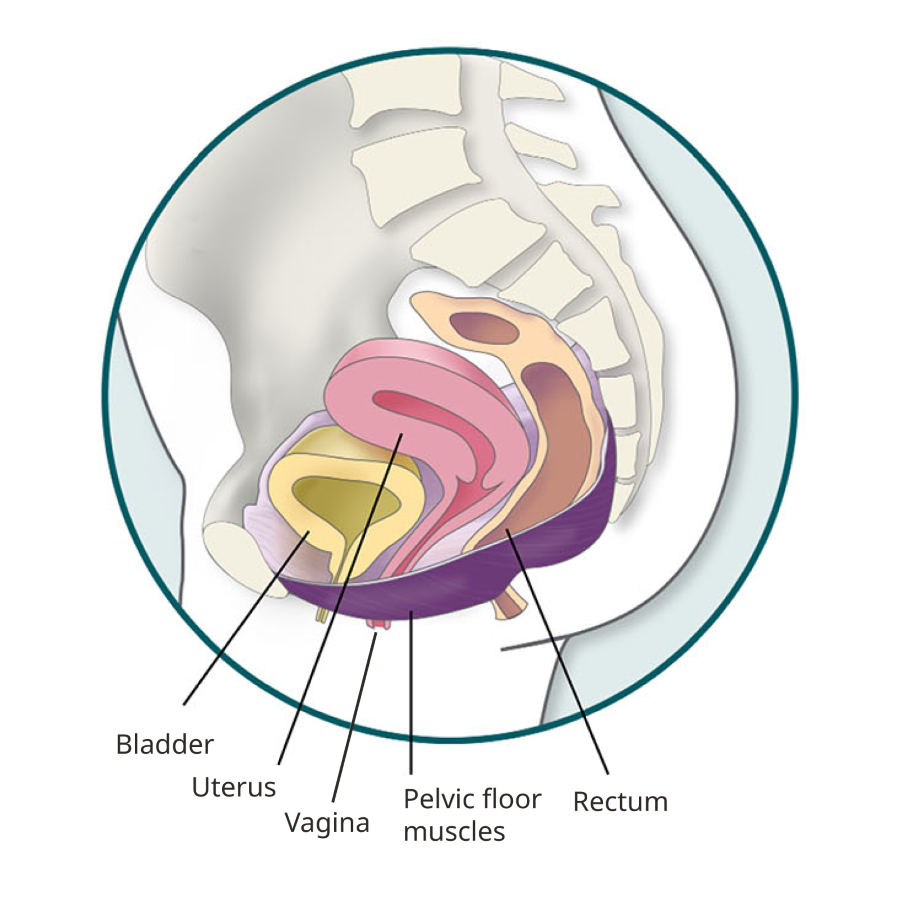
Pelvic organ anatomy
Types of pelvic prolapse
Bladder prolapse (cystocele): Your bladder falls onto your vagina, creating a bulge. It may cause urinary leakage, difficulty starting your flow, or trouble emptying your bladder. This is the most common type of prolapse.
Rectocele: Your rectum presses into your vaginal wall, making it hard to start or complete bowel movements.
Uterine prolapse (or vaginal vault prolapse): Your uterus drops into your vagina and creates a bulge. If your uterus has been removed, the top of your vagina collapses into the lower part. It may affect your bowel or bladder function or give you a feeling of pressure on your pelvic floor.
Enterocele: The vaginal skin is weak, allowing your small intestine to drop into the space of your vagina. This sometimes happens along with other types of prolapse.
What causes pelvic organ prolapse?
It is normal for the muscles and connective tissues in your pelvic floor to relax as you get older. Sometimes they become so weak, stretched or torn that your pelvic organs start to slip out of place. Doctors often don’t know why it happens. Aging, injuries, menopause and having a baby make it more likely.
Who gets pelvic organ prolapse?
About half of all women will experience some degree of pelvic prolapse during their lifetime. For most, the symptoms are mild. In about 3% of women, prolapse causes enough discomfort or disruption to need treatment.
Prolapse is most common in older women and in white and Latina women. It can also run in families.
Risks for women include:
- Pregnancy and vaginal childbirth
- Aging and menopause
- Injuries from childbirth, surgery, falls, radiation, or accidents
- Chronic pelvic pressure from obesity, heavy lifting, coughing or constipation
- Smoking
- Pelvic surgery, like a hysterectomy to remove your uterus
- Nerve and muscle disorders
Symptoms
Most women with mild prolapse do not have symptoms. If you have more serious prolapse, your symptoms may include:
- Discomfort, pressure or fullness in your vagina or pelvis
- Urinary leaks or frequent urination
- Trouble starting your urine flow or completely emptying your bladder
- A bulge of tissue coming out of your vagina
- Constipation or trouble completing bowel movements
- Pain in your lower back
- Difficulty using tampons
- Bleeding or sores in your vagina
- Painful sex
Diagnosing pelvic prolapse
We check your entire pelvic floor to find your type and degree of prolapse. We also check for any related bladder or bowel problems with the latest tests and imaging.
Your care team will talk with you about your options and explain each test. These may include:
Urodynamics: If you have urinary symptoms, we may suggest a series of tests to measure the pressure and muscle strength in your bladder.
Cystoscopy: We look inside your bladder using a lighted flexible telescope to check for problems.
Ultrasound: We are a leader in using high definition, 3D ultrasound imaging to check for pelvic floor disorders. Ultrasound uses sound waves to create moving images of your organs. We place a probe on the outside of your abdomen or near your vagina and anus.
Pelvic organ prolapse treatments
We build your care plan based on your condition and preferences. We offer the safest and most effective treatment options available. Your care team will talk with you about the best plan for you.
Non-surgical treatments
Pessary: A vaginal pessary is a removable device you can place in your vagina to lift and support your pelvic organs. Pessaries come in different sizes and are made of flexible materials like rubber. They can help most women with prolapse. We will help you choose the right pessary for you and make sure it fits, stays in place, and offers relief.
Estrogen therapy: Lower levels of this hormone after menopause can weaken your vaginal tissues. Taking estrogen may help strengthen them. Some women should not use estrogen. Your practitioner will talk to you about your potential risks and benefits.
Physical therapy with biofeedback: Our physical therapists can help you strengthen specific pelvic muscles with Kegel exercises. We can make sure you’re targeting the right muscles with biofeedback devices. As you perform an exercise, sensors on your vagina, rectum or skin monitor the strength of each squeeze. You see your results on a computer screen.
Surgical treatments
Our surgeons have the most experience and skill in Oregon and Southwest Washington correcting prolapse with the latest minimally invasive techniques.
We do many procedures using the da Vinci Surgical Robot. The robot helps your surgeon work through a few tiny incisions. That means less pain, less scarring and a faster recovery.
The decision to have surgery depends on your type of prolapse. It also depends on your age, activity level and overall health. If you have multiple pelvic floor disorders, we try to fix all the problems at one time.
Surgical procedures include:
Sacrocolpopexy: Your surgeon lifts and attaches your vagina to your tailbone using a piece of surgical mesh. It corrects prolapse of the uterus and vagina.
Uterosacral or sacrospinous ligament fixation: The surgeon stitches the top of your vagina to strong bands of tissue near the bottom of your spine. It provides more support for your vagina if you have a prolapsed uterus or vagina.
Anterior colporrhaphy: For some cystoceles (bladder prolapse), we need to lift and strengthen the front wall of your vagina to support your bladder. The surgeon makes an incision in the vaginal wall and stitches together stronger layers of tissue.
Posterior colporrhaphy: This procedure strengthens the back wall of your vagina to correct a rectocele. The surgeon cuts the vaginal tissue near the rectum and then creates a stronger barrier with stitches.
Enterocele repair: We strengthen your vaginal wall near your small intestine. The procedure is similar to a colporrhaphy.
Hysterectomy: We may surgically remove your uterus to treat severe uterine prolapse. This procedure can be done with minimally invasive surgery.
Obliterative vaginal procedures (colpocleisis): If you no longer want to have vaginal sex, we may recommend a procedure to shorten and close your vagina. We leave a small opening that does not affect your ability to pee, but it is too narrow for sex. This safe and effective surgery allows your vagina to support your pelvic organs and brings long-term symptom relief.
Resources about pelvic organ prolapse
- Pelvic Organ Prolapse: An Overview, U.S. National Library of Medicine
- Pelvic Organ Prolapse, Voices for PFD
- Pelvic Organ Prolapse, National Association for Continence
- Pelvic Organ Prolapse, Office on Women’s Health, U.S. Department of Health & Human Services
- Pelvic Organ Prolapse Videos, The American College of Obstetricians and Gynecologists
- Pelvic Support Problems, The American College of Obstetricians and Gynecologists
For patients
Call 503-418-4500 to make an appointment.
Location
OHSU Center for Women’s Health, Marquam Hill
Kohler Pavilion, seventh floor
808 S.W. Campus Drive
Portland, OR 97239
Free parking for patients and visitors
Refer a patient
- Refer your patient to OHSU.
- Call 503-494-4567 to seek provider-to-provider advice.
FAQ and Resources
Find answers to common questions and links to national resources.