Enlarged Prostate

Enlarged prostate, also called benign prostatic hyperplasia or BPH, is a common and highly treatable condition.
We provide:
- An expert team of urology specialists.
- Full evaluation for patients whose BPH has not responded to medications or treatment.
- A range of procedures, including Aquablation and UroLift.
- Care at multiple Portland locations.
Understanding enlarged prostate
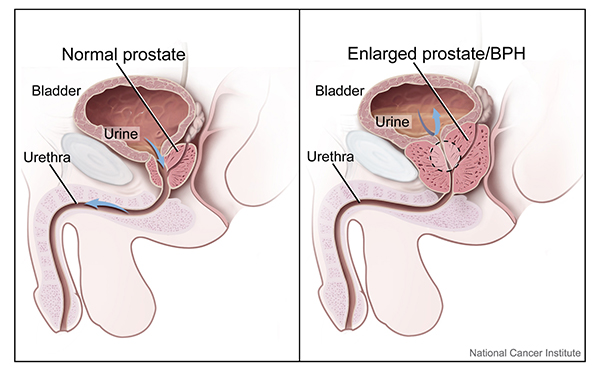
The prostate is a walnut-shaped gland, about the size of a pingpong ball, that sits between the bladder and penis. The prostate’s main role is to create the fluid in semen.
A narrow tube called the urethra runs from the bladder through the prostate to the penis. Urine and semen move through the urethra to leave the body.
The prostate tends to grow as you age. As it grows, it can press on or block the urethra. This condition is called enlarged prostate or benign prostatic hyperplasia.
Enlarged prostate (benign prostatic hyperplasia)
Symptoms of enlarged prostate
Storage symptoms:
- Having to urinate:
- Often during the day.
- Urgently.
- Several times overnight.
- Not being able to get to a toilet without urine leaking (urge incontinence).
Emptying symptoms:
- Feeling as if you have to strain or push on the bladder to urinate.
- Having trouble starting or maintaining the urine stream.
- Not emptying the bladder fully.
- Weak urine stream.
- In extreme cases: not being able to urinate.
Other symptoms:
- Blood in the urine
- Urinary tract infection
Risk factors for enlarged prostate
- Being older than 50.
- Having a family history of BPH or prostate cancer.
- Having certain conditions, such as type 2 diabetes, heart disease or obesity.
- Being physically inactive.
- Not being able to have an erection (erectile dysfunction).
For patients
New patients may need a provider’s referral to see us.
- Questions or appointments: 503-346-1500
- See our patient forms
Locations
OHSU Health Urology at Adventist Health Portland
10000 S.E. Main St., East Pavilion, Suite 260
Portland, OR 97216
OHSU Urology Clinic, South Waterfront
Center for Health & Healing, Building 1
3303 S. Bond Ave., 10th floor
Portland, OR 97239
Free parking for patients and visitors
Refer a patient
- Use our referral form
- Get provider-to-provider advice: 503-494-4567
Our services
You may need a provider’s referral to see us. Please check with your insurer.
Evaluation
You’ll need to come to your first visit with a full bladder so we can test:
- How long it takes you to urinate.
- How strong your urine flow is.
- Whether your bladder empties all the way.
We’ll discuss:
- Symptoms
- Diagnosis
- Medications and other treatments you have tried
- Procedures
Imaging
After your evaluation, we may have you return for imaging:
- A cystoscopy looks at the prostate and bladder. We put a tiny camera into the urethra to evaluate the urethra and bladder.
- An ultrasound measures the prostate. We put a probe that uses sound waves into the rectum.
- For patients with certain conditions: Videourodynamics is a test of how the bladder works. We put one pressure sensor in the bladder and another in the rectum. The sensors check the health of the bladder while it fills. They check whether it contracts properly to push out urine.
Treatments
We aim to provide the least invasive care that gives you the most relief.
Aquablation relieves symptoms for three or more years. It uses a robot-guided water jet to remove excess prostate tissue. Our surgeons do this procedure at the OHSU Health Urology clinic at Adventist Health Portland.
The procedure takes a half-hour to an hour, plus an overnight hospital stay. You will need a catheter for one to seven days. The time will depend on the size of your prostate and how much your bladder empties after the procedure. You can resume most activities in two to four weeks.
GreenLight uses a laser to remove excess prostate tissue, relieving symptoms for five or more years. It takes an hour to an hour and a half. You probably won’t need a catheter, and you can resume most activities in a week.
Prostatectomy at OHSU uses robotic surgery to remove the inner core of the prostate. It relieves symptoms permanently for most people.
Prostatectomy takes three to four hours, plus a one- or two-night hospital stay. You’ll need a catheter for seven to 10 days, and can resume most activities in four to six weeks.
Rezum Water Vapor Therapy relieves symptoms for up to five years. It uses a needle to inject steam into the prostate to remove excess tissue. The injection may be repeated several times.
It takes up to 10 minutes, and you’ll need a catheter for a few days. You can resume most activities in a few days.
TURP relieves symptoms for 15 or more years. It uses a device called an electrocautery loop to remove excess prostate tissue.
The procedure takes an hour to an hour and a half. Some patients stay in the hospital overnight. You’ll need a catheter for a day. You can resume most activities in four to six weeks.
UroLift implants titanium clips that hold excess prostate tissue away from the urethra. It relieves symptoms for five or more years.
It takes five to 30 minutes. You may need a catheter for a day, and you can resume most activities in a few days.
Sometimes the best or only treatment for BPH is a catheter, a flexible tube that empties the bladder into a toilet or collection bag. We can connect you to nursing services to help you manage your catheter.
- Intermittent catheter: You insert a fresh catheter into the penis several times a day.
- Indwelling catheter (Foley catheter): You have a catheter inserted into the bladder through the penis. On the bladder end, a water-filled balloon keeps the catheter in place. The catheter is changed every few months.
- Suprapubic catheter: You have a catheter placed in your bladder through a hole in the belly. The catheter is changed every four to six weeks.
Follow-up and side effects
We see you about a month after treatment to check how you’re healing and to see if your symptoms are better. It can take several weeks for symptoms to ease.
Depending on your treatment, you may have side effects for a few weeks that can include:
- Blood or bits of tissue in urine.
- A mild burning sensation when you urinate.
- Having to urinate often or urgently (overactive bladder).
- Leaking urine (incontinence).
- Ejaculating semen into the bladder rather than through the penis (dry orgasm).
- Not being able to have an erection (erectile dysfunction).
- Urinary tract infection.