Uterine Sarcoma
Uterine sarcoma is a complex condition that requires skillful care from a team of specialists. Our expertise includes:
- Highly trained doctors with years of experience treating patients with gynecologic cancers.
- A team approach, in which experts from different medical fields pool their knowledge for your benefit.
- Access to promising experimental treatments through our clinical trials.
- A wide range of support services.
- Options to protect your fertility.
Links
Understanding uterine sarcoma
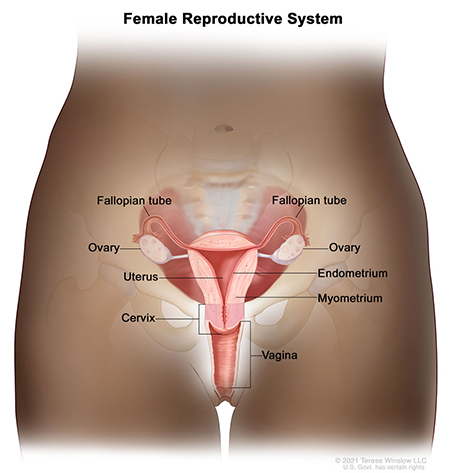
Uterine sarcoma is a rare type of cancer that starts in the uterus, the small, pear-shaped organ inside the pelvis. Sometimes cells start to divide and multiply out of control, forming tumors. When these tumors occur in muscle or connective tissue, they are known as sarcomas.
Uterine sarcoma may occur in:
- The muscles of the uterus, also known as the myometrium.
- The layer of connective tissue that surrounds and supports the uterus, also known as the parametrium.
Uterine sarcoma is very rare. The American Cancer Society estimates that about 3,300 cases are diagnosed in the United States every year. Most cases are found in people over 40. The average age at diagnosis is 60.
Doctors don't yet know what causes it, but they have identified risk factors. You’re more likely to get it if:
- You’ve had radiation therapy to treat cancer in the pelvic region.
- You’ve had a type of eye cancer called congenital retinoblastoma.
- Your family has a history of a type of kidney cancer called hereditary leiomyomatosis and renal cell cancer. OHSU offers genetic counseling, risk assessment and testing to see if you have inherited a gene linked to a higher risk.
- You’re taking tamoxifen for breast cancer.
Survival rates
Uterine sarcoma is an aggressive type of cancer. It is often found in later stages, making it tougher to treat.
A key concept in understanding survival is five-year relative survival rate. This is the percentage of people who will be alive five years after they were first diagnosed compared with those who don’t have the cancer. (It doesn’t count death from other causes.)
The five-year relative survival for uterine sarcoma is 75% for patients whose cancer is found early, according to a study from 2023.
Outcomes for later stages are discouraging. It’s important to remember that survival rates are averages, and don’t predict the outcome for any one person. They are also based on treatments that were available five years ago.
The good news is that survival rates for uterine sarcoma are getting better, especially when it’s caught early. Researchers are hard at work to find new ways to help patients with this condition.
Symptoms
- Unusual vaginal bleeding not related to menstruation
- Vaginal bleeding after menopause
- A mass in the vagina
- Pain or a feeling of fullness in the abdomen
- Frequent urination
For patients
- Request an appointment
- Seek a second opinion
- Ask questions
Location
Knight Cancer Institute, South Waterfront
Center for Health & Healing, Building 2
3485 S. Bond Ave.
Portland, OR 97239
Free parking for patients and visitors
Refer a patient
- Refer your patient to OHSU.
- Call 503-494-4567 to seek provider-to-provider advice.
Cancer clinical trials
Clinical trials allow patients to try a new test or treatment.
Read more
Learn more about OHSU Knight Cancer Institute treatments:
Stay informed
News: Read about research breakthroughs, patient care and many other topics on our OHSU News site.
Connect with us
Diagnosis
If you have symptoms, your doctor will ask you about your health history and do a physical exam. They will also most likely do a pelvic exam.
These are other tests your care team may recommend:
- Transvaginal ultrasound: Your provider inserts a small wandlike device into your vagina. The device produces sound waves that create an image of your uterus. This can show something unusual in the lining.
- Hysteroscopy: Your provider inserts a thin, flexible tube through your vagina and cervix into your uterus. The device has a tiny camera that shows the uterus lining.
- Endometrial biopsy: Your provider inserts a thin, flexible tube into the uterus through the vagina and cervix. Suction is used to extract a tiny bit of the endometrium. We examine the tissue under a microscope to look for cancer cells.
- Dilation and curettage: This procedure is also called D&C. It’s sometimes needed if a biopsy sample doesn’t provide clear results. Your doctor temporarily expands the opening of the cervix. They use an instrument to scrape tissue from inside the uterus.
- Genetic testing: Your doctor may recommend a blood test to look for changes in your DNA that are linked to uterine sarcoma. This information can help guide your care plan.
- Pap test: Unfortunately, Pap tests are not useful in detecting uterine sarcoma.
Types of uterine sarcoma
- Uterine leiomyosarcoma: This type starts in the muscle wall of the uterus, known as the myometrium. It is the most common type of uterine sarcoma.
- Adenosarcoma: This type starts between two layers of cells: the endometrium, which lines the inner wall of the uterus, and the myometrium, which surrounds the endometrium. It accounts for about 5% of uterine sarcomas.
- Endometrial stromal sarcoma: This type starts in the stroma, a layer of connective tissue that supports the endometrium. It tends to grow slowly, making it easier to treat. It accounts for about 2% of uterine sarcomas.
- Undifferentiated sarcoma: The cells in this type all look the same. This type accounts for about 5% of uterine sarcomas.
Stages of uterine sarcoma
The stage of your cancer describes its size and spread. This helps your team plan the best treatment. The stage also reflects the grade of your cancer (how normal or abnormal the cancer cells look under a microscope) and other factors.
This is the staging system for leiomyosarcoma and endometrial stromal sarcoma.
Stage I: Cancer is only in the uterus.
- Stage IA: The tumor is 5 centimeters or less in diameter.
- Stage IB: The tumor is more than 5 centimeters.
Stage II: Cancer has spread beyond the uterus but remains inside the pelvis.
- Stage IIA: The tumor has spread to the ovaries, fallopian tubes or ligaments.
- Stage IIB: The tumor has spread to other tissues inside the pelvis.
Stage III: Cancer has spread to the abdomen.
- Stage IIIA: The tumor has spread to another site.
- Stage IIIB: The tumor has spread to more than one site.
- Stage IIIC: The tumor has spread to more than one site and to lymph nodes.
Stage IV: Cancer has spread to the bladder, rectum or other parts of the body.
- Stage IVA: The tumor has spread to the bladder or rectum.
- Stage IVB: The tumor has spread to distant parts of the body.
Treatment
Your care team will work with you to develop a treatment plan. Here are some options:
Surgery is the frontline treatment for uterine sarcoma. Our doctors use minimally invasive and precise robotic surgical techniques. This allows for less pain, smaller incisions and quicker recovery.
Options include:
- Total hysterectomy, which removes the uterus and cervix.
- Bilateral salpingo-oophorectomy, which removes ovaries and fallopian tubes on both sides.
- Radical hysterectomy, which removes the uterus, cervix, part of the vagina and possibly the ovaries, fallopian tubes and nearby lymph nodes.
- A lymph node dissection, which removes lymph nodes so they can be checked for cancer cells.
- Find out how we use surgery to treat cancer.
Radiation therapy uses beams of energy to damage or destroy cancer cells. We may recommend two types of therapy for uterine sarcoma:
- External beam radiation, which uses a machine outside the body to target the cancer.
- Brachytherapy, which generates a higher dose in a smaller area. A radiation source is placed in a tube that’s inserted into the vagina for a short time. You may get several doses in a series of visits to the clinic.
Chemotherapy drugs are used to kill or stop the growth of cancer cells. The drugs are usually given in a series of infusions — slow IV drips. They may be used along with surgery or radiation therapy.
Hormone therapy removes, blocks or stimulates hormones to stop certain cancer cells from growing. These drugs may be given as a pill, liquid or shot.
These drugs harness the power of your immune system to knock out cancer cells. They prime immune cells to seek out and target cancer cells.
Targeted therapy drugs lock onto cancer cells and shut them down, minimizing damage to healthy cells. Targeted therapy is not often used in uterine sarcoma.
Support for you and your family
- Look for an OHSU clinical trial for uterine sarcoma.
- Learn about options to protect your fertility.
- We offer the area’s only program to support the sexual health of women affected by cancer.
- Read about OHSU’s cancer registries, including one for sarcoma survivors.
Learn more
- Uterine Sarcoma, National Cancer Institute
- Uterine Sarcoma, American Cancer Society
- Uterine Cancer, Society of Gynecologic Oncology