Clinical Program
The blood-brain barrier (BBB) consists of a layer of endothelial cells that line the blood vasculature throughout the brain. This layer is held together by tight junctions that prevent small molecules from diffusing through the gaps between the cells, the so-called paracellular route. Because diffusion of molecules across the cells by other means, pinocytosis for example, is minimal, it is these tight junctions and their inherent impermeability to water soluble molecules, or molecules larger than 200-400 daltons, that creates the blood-brain barrier. Dr. Neuwelt's research paper "Mechanisms of Disease: The Blood Brain Barrier" (Neurosurgery, January, 2004) is available on request.

Blood vessels in human brain. A plastic emulsion was injected into brain vessels and brain parenchymal tissue was dissolved. (photo on left).
Zlokovic & Apuzzo: Neurosurgery 43(4):877-878, 1998. (provided by permission from Lippincott Williams & Wilkins)
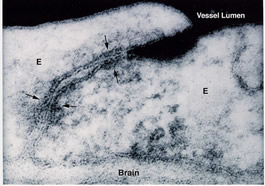
The electron micrograph (on the right) shows electron dense lanthanum (dark areas in vessel lumen) unable to penetrate beyond a tight junction (arrow) between endothelial cells (labeled E).
(provided courtesy Dr. Milton Brightman at the NIH)
Blood-Brain Barrier Opening
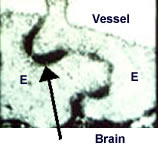
Permeability of the BBB after blood-brain barrier disruption (BBBD) is shown by the electron micrograph of peroxidase staining (indicated by arrow) between endothelial cells (labeled E).
(provided courtesy Dr. Milton Brightman at the NIH)
Intracarotid or intravertebral infusion of hyper osmotic saccarides (e.g. mannitol) leads consistently to a reversible opening of the barrier. This successful and noninvasive way of introducing therapeutic agents in patients with brain tumors has the disadvantage of randomly disseminating potentially neurotoxic agents throughout the brain.
Although some studies have shown that the use of oral (Temodar) or intravenous (BCNU) adjuvant chemotherapy following surgery prolongs survival in a selected group of patients, these improvements have generally been modest, and the great majority of patients are not cured. Limited therapeutic success in the treatment of CNS neoplasia with chemotherapy is generally attributed to two factors: natural or acquired resistance to chemotherapy expressed by tumor cells, and delivery impediment related to the BBB. The goal of the BBBD procedure is to maximize the delivery of the chemotherapeutic agent to the tumor cells for a given systemically administered dose. This increase in delivery also serves the purpose of increasing the therapeutic index/toxicity ratio. It has been shown in preclinical animal studies that a marked increase in water-soluble agent concentration (10- to 100-fold) can be induced in the brain, tumor and CSF after osmotic BBBD and intra-arterial administration (Neuwelt 1998). Kraemer (2002), a statistician with the BBB program, has reviewed the importance of dose intensity in CNS tumor treatment.
While many chemotherapeutics exhibit excellent activity in vitro, their therapeutic efficacy is often significantly diminished when administered, since they are unable to gain access to the diseased sites at a sufficient concentration for an appropriate time. This problem is commonly encountered by neuro-oncologists in the treatment of both primary and metastasic brain tumors. The goal of intra-arterial infusion is to increase the therapeutic index of a compound that already demonstrates activity following its IV administration. The intra-arterial route is more advantageous than systemic (IV) drug administration (which includes direct IV, oral, intramuscular, subcutaneous, intraperitoneal and even inhalation whereby drug enters the venous system before reaching the brain) because of these factors:
- With intra-arterial infusion, the first circulation of the drug is through the brain. After the drug leaves the target and enters the systemic circulation its pharmacokinetics are similar to those following IV administration.
- With regards to the toxicity, numerous studies have clearly established this route, combined with osmotic disruption, is a safe and consistent treatment modality. Please see the Institute for Clinical Systems Improvement report on blood brain barrier disruption chemotherapy.
- An increase in concentration of the drug at the target site will result in an increase in activity if a maximal effect has not already been achieved (Kraemer 2002).
Drugs that are ideal for intra-arterial infusion must enter tumor cells and possess a short half-life. The hyperosmotic disruption technique is one of the most widely used methods to open the blood-brain-barrier. A 30 second continuous intra-arterial infusion of mannitol in a given circulation at a rate sufficient to fill the whole vascular tree of that circulation produces an osmotic gradient that draws free water from the endothelial cells and osmotically shrinks the cells. At present, in clinical assessment at multiple centers, its value in a variety of adult and pediatric brain tumors is being assessed. Additional techniques are based on different mechanisms and include bradykinin receptor-induced barrier permeability modification (RMP-7) as well as NO-induced changes in vasodilation of brain tumor capillaries.
Indications
Blood-brain barrier disruption (BBBD) is currently used clinically to increase the delivery of chemotherapeutic agents and in some cases monoclonal antibodies (mAb) for the treatment of brain tumors. Any central nervous system neoplasm with infiltrating features, chemo sensitivity, and potential to spread cells to the cerebrospinal fluid (CSF) has the possibility of being treated with intra-arterial chemotherapy with blood-brain barrier disruption. Please review the currently open studies at clinical trials.
Contraindications
The blood-brain barrier disruption technique is a physiologically stressful procedure. It produces a transient rise in intra-cranial pressure (ICP) from normal baseline values of 3 to 9 cm H2O to peaks of 16-23 cm at 30 minutes post disruption. This transient rise in ICP has been shown to correlate with a 1.5 percent increase in brain fluid content. In preclinical studies, this transient increase in ICP was not associated with any clinical sequelae (Neuwelt 1989). It illustrates, however, the rationale behind the very first contraindication of osmotic BBBD: the presence of significant mass effect.
Therefore, the following criteria must be used:
- Patients with radiological signs of intra-cranial herniation with associated rapid neurologic deterioration are ineligible.
All other patients displaying significant radiological signs of mass effect, but not strictly adhering to these two absolute contraindications, must be individually and carefully screened. In general, patients with significant mass effect will initially undergo intra-arterial chemotherapy infusion without BBBD until decrease in tumor bulk safely allows a disruption.
Other contraindications include:
- Patients with evidence of spinal cord block from tumor mass
- Patients who have an Eastern Cooperative Oncology Group (ECOG) performance score equal to or greater than 3
- Patients who are not expected to survive for more than 3 months from initiation of treatment
- Patients at significant increased risk for general anesthesia
- Patients who are pregnant
Clinical studies open to subject enrollment
Please see clinical trials for information and eligibility requirements for our open clinical studies.