Understanding Breast Cancer
Breast cancer is the most common cancer in women behind skin cancer. The good news is that 91% of breast cancer patients survive at least five years after diagnosis.
This overview is designed to give you an essential understanding of this complex condition. Your care team at OHSU will go over the specifics of your diagnosis and treatment options.
What is breast cancer?
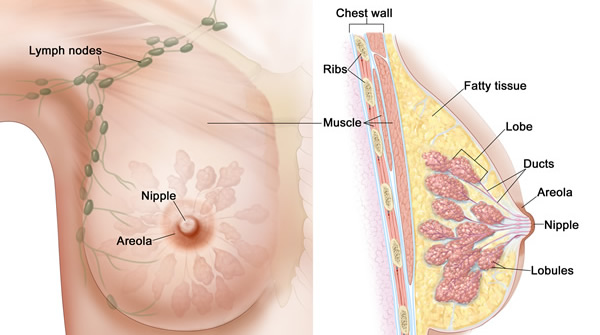
Breast cancer occurs when cells in the breast multiply out of control, forming clusters of cancer cells or a tumor. Breast cancer usually starts in:
- Lobules, the milk-producing glands.
- Ducts, the thin tubes that carry milk from the lobules to the nipples.
Who gets breast cancer?
The National Cancer Institute estimates that about 311,000 women in the U.S. will be diagnosed with breast cancer in 2024 . Overall, about one in eight women will be diagnosed sometime in her life. Almost four million U.S. women are living with or have survived breast cancer.
Men get breast cancer, too, but not as often. The American Cancer Society estimates that 2,800 men in the U.S. were diagnosed with breast cancer in 2023.
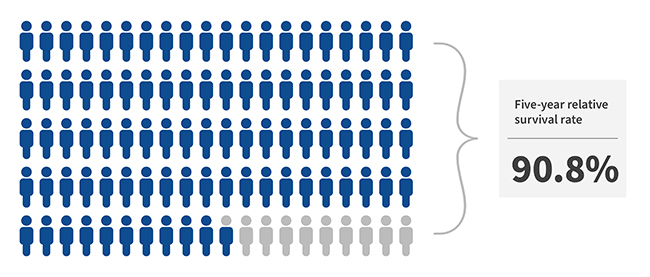
Breast cancer survival rates
On average, 91.2% of U.S. women with breast cancer survive at least five years after their diagnosis, compared with the general population. This is called the relative survival rate. It excludes the risk of dying from something else.
Among those whose cancer is found only in the breast, 99.6% survive at least five years.
These figures reflect significant strides in survival rates in recent decades. At the same time, they are averages, which can’t predict the outcome for any one woman. They also reflect the treatments that were available five or more years ago. You can find more statistics at the National Cancer Institute.
What causes breast cancer?
In 5% to 10% of cases, the disease can be traced to an inherited gene. Risk also increases with age, a family history of breast cancer, and other factors. In most cases, though, the cause is unknown. Most women in the high-risk group will not get breast cancer, and some women with no risk factors will.
Breast cancer symptoms
Symptoms of breast cancer vary greatly. It’s possible to have cancer with no symptoms. It’s also possible that a symptom has another cause and isn’t from cancer. If you do have cancer, early detection is important. Do a self-exam each month, and see your doctor if you notice any of the following:
- A lump or mass in a breast
- A lump, swelling or thickening in or near a breast or under your arm
- Dimpling or puckering of skin on a breast
- A nipple pulled to one side, pulled inward or inverted
- Red or scaly skin on a breast
- Orange peel texture on breast skin
- Change in breast size or shape
- New asymmetry of the breasts
- Nipple discharge
- Newly visible vein on the breast
Types of breast cancer
Breast cancer, though commonly considered a single diagnosis, is made up of several distinct conditions. Most breast cancers are carcinomas, meaning they arise in the “epithelial” cells that line the breast’s milk glands or ducts. Rarely, breast cancer can be a sarcoma, arising in the breast’s connective tissue.
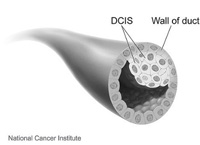
In this noninvasive condition, abnormal cells are found in the lining of ducts. DCIS is considered a precancer or precursor to cancer. “In situ” means the cells are in their original place and have not invaded beyond the duct walls or spread to other tissues.
DCIS is usually found on a mammogram and is highly treatable. Treatment is necessary, however, because some cases become invasive.
LCIS is an uncommon, noninvasive condition in which abnormal cells are found in the lobules, or milk-producing glands. It is not cancer but a marker of higher risk for cancer. “In situ” means the cells are in their original place and have not spread to other tissues.
LCIS usually requires no treatment. Because it puts women at higher risk of invasive breast cancer, though, monitoring is essential. LCIS is usually found after a biopsy (removal of tissue for examination under a microscope) for another breast condition. It may or may not show up on a mammogram.
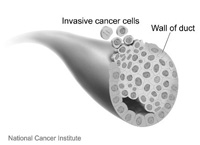
In invasive ductal carcinoma, cancer cells have broken through the duct wall and invaded nearby tissue.
This condition is also called infiltrating ductal carcinoma. This is the most common breast cancer diagnosis.
IDC subtypes
- Adenoid cystic breast cancer: The cancer cells in this rare type look like “adeno” (relating to glands) cells more common in salivary glands. It’s easier to treat than more common ductal cancers.
- Cribriform carcinoma of the breast: In this type, cancer cells cluster in the connective tissue between ducts and lobules. This type is highly treatable.
- Medullary carcinoma of the breast: This type is characterized by a soft tumor that looks like a part of the brain called the medulla. Despite cells that look aggressive, this type tends to be slower-growing and easier to treat.
- Micropapillary carcinoma of the breast: Cancer cells form clusters in this aggressive type.
- Metaplastic carcinoma of the breast: This very rare type contains a mixture of cell types and can be difficult to diagnose. It tends to be more aggressive than other types.
- Mucinous carcinoma of the breast: Cells in this type are surrounded by mucin, a main part of mucous. This type is less likely to spread and easier to treat.
- Papillary carcinoma of the breast: The cells in this rare type feature fingerlike extensions called “papules.” This type tends to affect older women and is usually easier to treat than other ductal cancers.
- Tubular carcinoma of the breast: This type involves tube-shaped structures called tubules. It tends to be less aggressive.
This condition, also called infiltrating lobular carcinoma, is the second most common breast cancer diagnosis after IDC. In ILC, cancer cells have spread from a lobule to surrounding tissue.
In this aggressive form of breast cancer, cancer cells block lymph vessels in the breast’s skin. This leads to swelling, redness and an orange-peel texture. It is often mistaken for a breast skin infection called mastitis.
This cancer tends to spread rapidly, making prompt treatment essential. It also tends to strike younger women. It’s relatively rare, making up about 1% to 5% of U.S. breast cancer diagnoses.
In this form of breast cancer, also called Paget disease of the nipple, cancer cells affect the skin of the nipple and, usually, the surrounding areola. Patients often have one or more DCIS or invasive tumors in the affected breast. This condition makes up about 1% to 4% of U.S. breast cancer diagnoses.
Breast cancer is rare in men, making up less than 1% of diagnoses. Men who get breast cancer tend to be ages 60 to 70. Types that affect men are DCIS, IDC, inflammatory breast cancer and Paget disease of the nipple.
Having a family history of breast cancer and/or a genetic mutation that increases the risk of breast cancer are among risk factors. Most often, male breast cancer is diagnosed after a lump is felt. Tests, staging, treatment and survival rates are similar to those for women.
Breast tumors are rare in children. Even when they occur, they are almost always benign (not cancer).
- Breast sarcoma: This rare, aggressive type develops in the breast’s connective tissue. It behaves differently than other breast cancers. Surgically removing the tumor is especially important.
- Mixed carcinoma of the breast: This cancer develops where a duct and lobule meet, resulting in cancer that contains both ductal and lobular cancer cells. It’s also called invasive mammary breast cancer or infiltrating mammary breast cancer. Outcomes are similar to those for IDC.
- Phyllodes tumors of the breast: These rare, fast-growing tumors develop in the breast’s connective tissue, most often in women in their 40s. Most of the time, they are benign (not cancer). They can also be malignant (cancer) or borderline — a mix of benign and malignant. The name comes from a Greek word for “leaf,” named for the pattern the cells form.
- Secondary tumors: In rare cases, a breast tumor is cancer that has spread from elsewhere in the body. “Secondary” means it’s not the “primary,” or main, tumor.
The role of lymph nodes in breast cancer
Lymph nodes are small bean-shaped glands found throughout the body. They are part of the lymphatic system, which circulates a clear fluid through the body to fight illness. Lymph nodes filter the fluid and can trap cancer cells. If breast cancer spreads, it shows up in nearby lymph nodes first.
This is why, if you have invasive breast cancer, your lymph nodes will be checked for cancer cells. Tissue can be extracted with a needle in a procedure called a needle biopsy, or nodes can be removed in surgery. If cancer cells are found, additional treatment may be recommended.
Breast cancer stages
Your care team will assign a stage to your cancer, such as Stage 0, Stage I, Stage II, and so on. The stage indicates how advanced your cancer is and whether it’s likely to grow slowly or quickly. This helps doctors plan the most effective treatments.
Stage depends on:
- The size of any tumor.
- Any spread to lymph nodes.
- Any spread to other body parts.
- The cancer's receptors, if any.
- The cancer's grade.
- For some tumors, how likely the cancer is to recur and how likely it is to respond to certain treatments.
Generally, higher-stage cancers require more aggressive treatment. This is only one element that goes into deciding treatment options, however. Age, family history, general health and other factors are also important.
Stage is determined using:
- Physical exam
- Imaging, such as a mammogram or MRI
- Biopsy of a tumor or lymph nodes (extracting tissue with a needle or as part of surgery so it can be analyzed under a microscope and tested)
- For certain tumors, analysis of the cancer's genetic characteristics (genomic analysis)
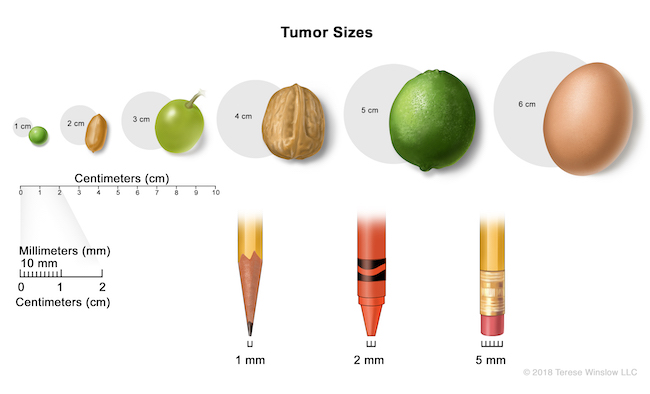
Because breast cancer staging has so many variables, it's highly complex. Here's a simple outline to show the stages. Find complete information at breastcancer.org.
Stage 0: Cancer cells are found only in a duct. This is also called carcinoma in situ, or cancer in its original place. (LCIS, considered a benign condition, is not included in staging.)
Stage I: The cancer is invasive and has spread outside a duct or lobule. Cancer is in the breast and/or lymph nodes. The cancer has at least one receptor. Stage I is divided into stages IA and IB.
Stage II: Cancer is more likely to have spread to lymph nodes, such as nodes under the arm. It's less likely to have receptors than in stage I. Stage II is divided into stages IIA and IIB.
Stage III: The breast tumor is more likely to be larger compared with stages I and II, and the cancer is more likely to have spread to lymph nodes or to more lymph nodes. The cancer is also more likely to be higher grade and/or to have no or fewer receptors. It may have grown from the breast into the chest wall. Stage III is divided into stages IIIA, IIIB and IIIC.
Stage IV: The cancer has spread to another part of the body, such as the bones, liver, lungs or brain.
Localized, regional or distant
This is another way of describing a breast cancer’s stage.
Localized: This cancer has not spread outside the breast.
Regional: The cancer has spread to nearby lymph nodes or other tissue.
Distant: The cancer has spread to other parts of the body, such as the bones, liver, lungs or brain.
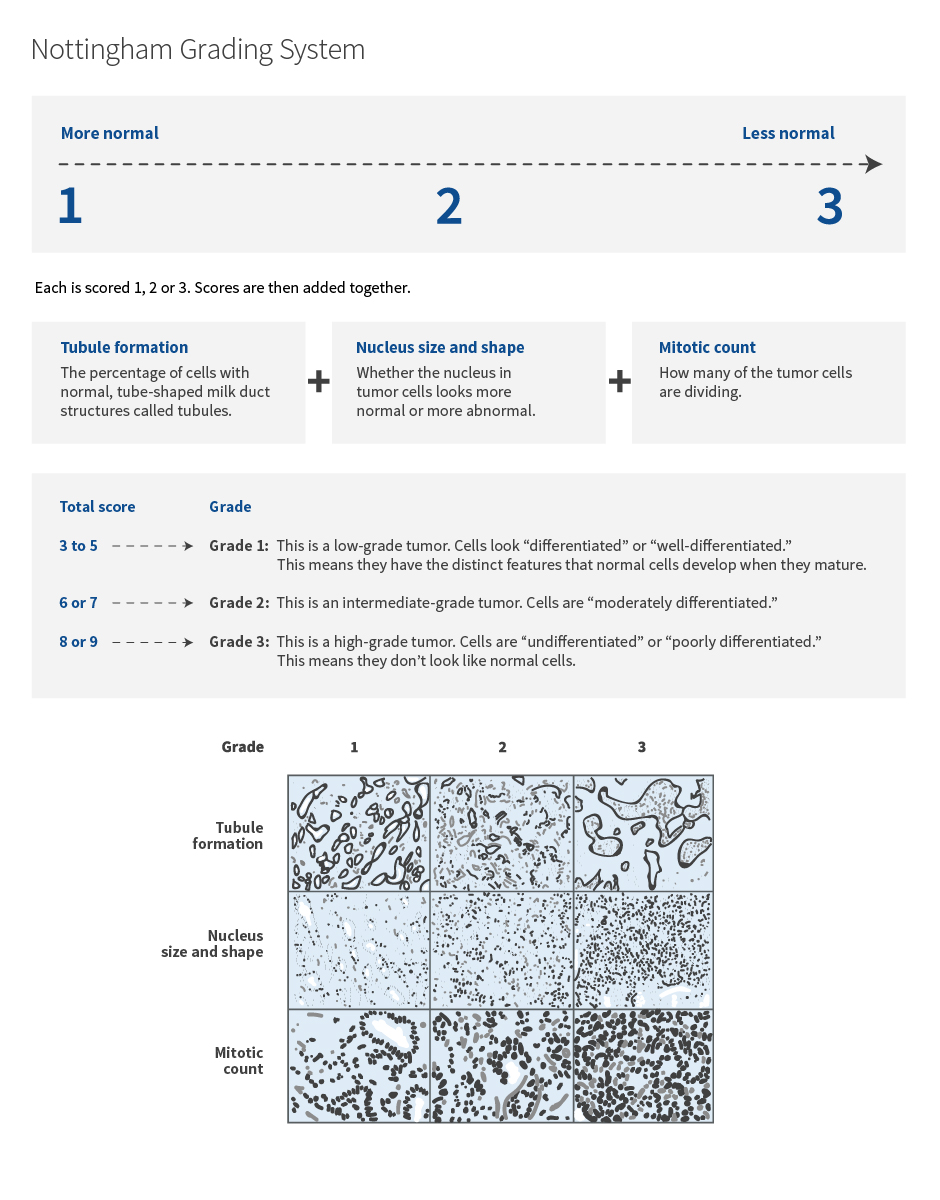
Breast cancer grades
A doctor called a pathologist determines a tumor’s grade by looking at samples under a microscope. Higher-grade tumors are generally more likely to grow and spread, requiring more aggressive treatment. For breast cancer, the Nottingham grading system is most common.
Receptor status
Breast cancer cells often have a type of protein called a receptor. Receptors are like locks. Medications or substances in the body can fit into them like keys, telling the cells how to behave.
For example, a hormone in the body might “bind” (fit in the lock) to a receptor and tell the cancer cell to grow. A medication can fight the cancer by lowering the amount of that hormone in the body. Or a medication might bind to the receptor, preventing the hormone from delivering its instructions.
Your cancer will be tested for three receptors. The first two are “hormone” receptors:
- Estrogen receptors
- Progesterone receptors
- HER2 receptors
Your cancer can test positive for one, two or all three receptors. If your cancer has no receptors, it’s called “triple negative.”
Hormone receptors
Hormones are chemicals in the body that control functions such as growth. Breast cancer can have receptors for two hormones — estrogen and progesterone.
In women, estrogen regulates the development of breasts and menstruation, among other things. Progesterone prepares the uterus for pregnancy and helps regulate menstrual cycles.
Tests determine if your cancer is positive or negative for each receptor. If it’s positive, medication may affect the cancer. These abbreviations are used:
- ER+ (estrogen receptor positive)
- ER- (estrogen receptor negative)
- PR+ (progesterone receptor positive)
- PR- (progesterone receptor negative)
HER2 receptors
HER2 stands for “human epidermal growth factor receptor 2.” HER2 is a gene that makes HER2 proteins, or receptors. The receptors regulate cell growth and division.
In some breast cancers, the HER2 gene makes too many copies of itself (amplification), resulting in too many HER2 receptors (overexpression). This causes cells to grow and multiply out of control.
If tests show that your cancer has this, it’s called HER2 positive or HER2+. If not, it's HER2 negative or HER2-.
A medication called Herceptin can bind to the HER2 receptors to prevent them from receiving the chemical signals to grow and multiply. Herceptin can also tell the immune system to destroy the cells it binds to. Other medications can also use the HER2 receptor to fight cancer.
Learn more
- Breastcancer.org
- Breast Cancer, National Cancer Institute
- Breast Cancer, American Cancer Society
- Basic Information About Breast Cancer, Centers for Disease Control and Prevention
- Breast Cancer, MedLinePlus, National Library of Medicine
- National Breast Cancer Foundation
- About Breast Cancer, Susan G. Komen
- Male Breast Cancer Treatment, National Cancer Institute
For patients
Call 503-494-4673 to:
- Make an appointment
- Seek a second opinion
- Ask questions
Location
OHSU Breast Center, South Waterfront
Center for Health & Healing, Building 2, ninth floor
3485 S. Bond Ave.
Portland, OR 97239
Free parking for patients and visitors
Refer a patient
- Refer your patient to OHSU.
- Call 503-494-4567 to seek provider-to-provider advice
Cancer clinical trials
Clinical trials allow patients to try a new test or treatment.
Read more
Learn more about OHSU Knight Cancer Institute treatments: